Endometriosis and polycystic ovary syndrome (PCOS) are two distinct gynaecological conditions with differing causes and symptoms. While endometriosis involves the growth of uterine-like tissue outside the uterus, causing pain and potential fertility issues, PCOS is characterised by hormonal imbalances leading to irregular menstrual cycles, cysts on the ovaries, and often, challenges with fertility.
In this article, we delve into the intricate world of women’s health, unravelling the complexities of two prevalent conditions: endometriosis and polycystic ovary syndrome (PCOS). Both conditions, often misunderstood and misdiagnosed, significantly impact the lives of many women. Yet, they are distinct in their causes, symptoms, and treatments.
Understanding PCOS and Endometriosis
Endometriosis and polycystic ovary syndrome are two significant conditions affecting women’s reproductive health, particularly during their reproductive age. Endometriosis occurs when endometrial tissue, similar to the lining inside the uterus, grows outside it, often resulting in chronic pelvic pain, abnormal tissue growth, and excessive bleeding. This condition can lead to severe pain during menstrual cycles and can even affect the fallopian tubes and other parts of the pelvic cavity.
On the other hand, PCOS is a hormonal disorder characterised by insulin resistance, weight gain, and an imbalance in male hormones. The first signs of PCOS are irregular periods, multiple cysts on the ovaries (polycystic ovarian syndrome), and excess hair growth (also known as hirsutism). It is often diagnosed through blood tests, pelvic exams, and the presence of similar symptoms related to the menstrual cycle.
Both conditions, while having some overlapping symptoms like menstrual irregularities and pelvic pain, have distinct causes and manifestations. Endometriosis involves the growth of endometrial cells outside the uterus, possibly due to factors like retrograde menstruation or endometrial cell transport. In contrast, PCOS is more linked to hormonal imbalances and risk factors like family history and can manifest in different ways, including effects on the menstrual cycle and the appearance of the reproductive system on ultrasound.
It’s essential to understand these conditions, as they not only cause discomfort but also pose challenges for women of childbearing age, particularly in terms of fertility. Diagnosing each condition – whether through recognising endometriosis symptoms or confirming a PCOS diagnosis – is essential for effective management and treatment, including options like hormonal birth control for endometriosis or laparoscopic ovarian drilling for PCOS.
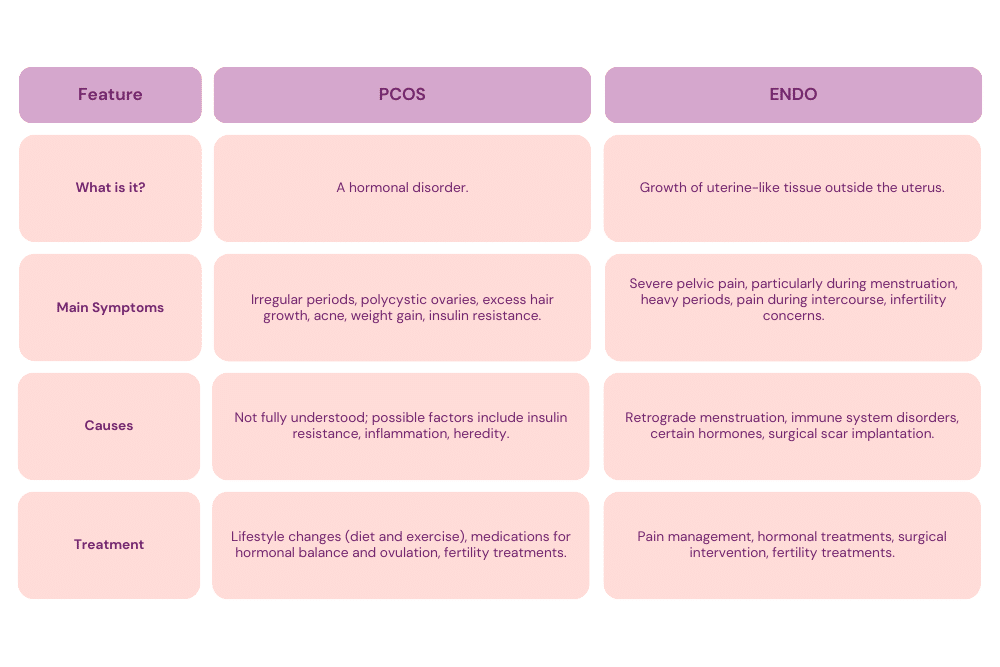
Endo vs. PCOS: What’s the Difference?
Endometriosis and polycystic ovary syndrome are both common conditions in women of reproductive age, but they have distinct differences in their origins, symptoms, and impacts on health.
Endometriosis is characterised by the presence of endometrial tissue, which normally lines the uterus, growing outside the uterus. This can lead to severe pelvic pain, especially during menstrual cycles, and can cause endometrial cells to affect other pelvic organs. The primary endometriosis symptoms include chronic pelvic pain, excessive menstrual bleeding (learn how to make your period lighter), pain during intercourse, and, in some cases, infertility. Endometriosis risk factors often include retrograde menstruation, where menstrual blood flows back through the fallopian tubes into the pelvic cavity, and a family history of endometriosis.
In contrast, PCOS is a hormonal disorder where the ovaries produce an excess amount of male hormones (androgens). This hormonal imbalance can lead to a range of symptoms, including irregular periods, multiple cysts on the ovaries, weight gain (explore how to lose weight with PCOS), insulin resistance, excessive hair growth, and acne. PCOS is often associated with an increased risk of developing other health issues like diabetes and heart disease. Unlike endometriosis, which primarily involves abnormal tissue growth, PCOS is more about the hormonal imbalance within the body and its effects on the reproductive system.
While both conditions can cause pelvic pain and impact fertility, their underlying causes, treatment approaches, and associated health risks differ significantly. For instance, hormonal birth control might be used to treat endometriosis, while lifestyle changes and medications to regulate insulin levels could be more relevant for PCOS management. Understanding these differences is vital for accurate diagnosis and effective treatment of each condition.
Can You Have Both PCOS and Endometriosis?
A woman can have both polycystic ovary syndrome and endometriosis, although they are separate conditions with distinct causes and symptoms. Having both conditions simultaneously can complicate diagnosis and treatment, as the overlapping symptoms might mask the presence of the other condition.
PCOS, a hormonal disorder, is characterised by insulin resistance, irregular menstrual cycles, and the development of cysts on the ovaries due to hormonal imbalances, particularly an excess of male hormones. These hormonal imbalances can lead to symptoms like weight gain, excessive hair growth, and acne. PCOS is also known to be a leading cause of infertility due to its impact on ovulation.
Endometriosis, on the other hand, involves the growth of endometrial tissue outside the uterus, leading to chronic pelvic pain, especially during menstrual periods, and potentially affecting fertility. It occurs when endometrial cells, which normally line the uterus, grow in other parts of the body, causing pain, inflammation, and scar tissue formation.
Women with both conditions might experience a range of symptoms, such as severe pelvic pain, irregular periods, and challenges with fertility. The coexistence of PCOS and endometriosis can make it harder to diagnose and treat each condition effectively. It’s essential for healthcare providers to consider the possibility of both conditions when a woman presents with symptoms like menstrual irregularities, pelvic pain, or difficulty conceiving.
The management of both PCOS and endometriosis typically involves a multi-faceted approach, including hormonal treatments, lifestyle changes, and, in some cases, surgery. The complexity of having both conditions necessitates a personalised treatment plan, considering the symptoms and severity of each condition.
How do I know if I have PCOS or Endometriosis?
Determining whether you have polycystic ovary syndrome or endometriosis can be challenging due to some overlapping symptoms. However, each condition has distinct signs that can help differentiate them.
For PCOS, the symptoms are often related to hormonal imbalances. Key indicators include irregular menstrual cycles, which can range from infrequent or prolonged periods to no periods at all. Other signs are related to elevated levels of male hormones (androgens), manifesting as excess hair growth (hirsutism), severe acne, and sometimes scalp hair thinning. PCOS can also lead to multiple cysts on the ovaries, visible through ultrasound exams. Additionally, women living with PCOS may experience weight gain, difficulty losing weight, and signs of insulin resistance, like darkening of the skin in certain areas.
Endometriosis, in contrast, is primarily characterised by severe pelvic pain, especially during menstrual periods. This pain can also occur during sexual intercourse, bowel movements, or while urinating. Menstrual issues in endometriosis include heavy menstrual bleeding or bleeding between periods. Unlike PCOS, endometriosis can cause significant pain during pelvic exams and may lead to fertility issues. It’s important to note that endometriosis cannot be confirmed through a simple ultrasound; it often requires a laparoscopy, a surgical procedure where a camera is inserted into the pelvis to look for endometrial tissue outside the uterus.
If you’re experiencing symptoms like irregular periods, pelvic pain, or unusual hair growth, it’s important to consult with a healthcare provider. They can conduct various tests to diagnose PCOS and endometriosis, including blood tests, pelvic exams, ultrasounds, and sometimes laparoscopy. Each condition requires a specific approach to treatment, so an accurate diagnosis is essential for effective management.
Is PCOS or Endometriosis Worse for Fertility?
Determining whether polycystic ovary syndrome or endometriosis is “worse” for fertility is complex, as both conditions affect fertility in different ways and to varying degrees. The impact on fertility largely depends on the individual’s specific circumstances and the severity of the condition.
PCOS primarily impacts fertility through hormonal imbalances that can interfere with the regular ovulation process. Women with PCOS often experience irregular or absent menstrual cycles, making it challenging to predict ovulation and conceive naturally. Additionally, the presence of multiple cysts on the ovaries and insulin resistance associated with PCOS can further complicate fertility. However, many women with PCOS can conceive with the help of treatments that stimulate ovulation, such as medication or lifestyle changes aimed at reducing insulin resistance.
Endometriosis, on the other hand, can affect fertility by causing physical changes in the reproductive system. The growth of endometrial tissue outside the uterus can lead to the formation of scar tissue and adhesions, which can obstruct the fallopian tubes or interfere with the ovaries and egg retrieval. Endometriosis can also create an inflammatory environment that might impact egg quality, fertilisation, and implantation. While endometriosis can significantly impact fertility, many women with the condition are still able to conceive, often with the help of fertility treatments like in vitro fertilisation (IVF) or surgery to remove endometrial growths.
Can Endometriosis Look Like PCOS on Ultrasound?
Endometriosis and PCOS present differently on an ultrasound, making it unlikely for endometriosis to be mistaken for PCOS in this type of imaging. PCOS is typically identified on ultrasound by the presence of multiple cysts on the ovaries, often described as having a “string of pearls” appearance due to numerous small follicles surrounding the ovary.
Endometriosis cannot be reliably diagnosed through ultrasound alone, as it involves endometrial-like tissue growing outside the uterus, which may not be visible on ultrasound. Endometriosis often requires laparoscopic surgery for definitive diagnosis, where direct visualisation of endometrial implants occurs, distinguishing it from the ovarian-focused changes seen in PCOS.
Can PCOS Turn Into Endo?
Polycystic ovary syndrome cannot turn into endometriosis. PCOS and endometriosis are distinct medical conditions with different causes and physiological processes.
While both conditions can co-occur in the same individual, one does not cause or turn into the other. They are separate entities with different pathologies and treatment approaches. It’s important for individuals with either condition to get an accurate diagnosis and appropriate treatment specific to their condition.
Managing PCOS and Endometriosis: Tips and Insights
Effectively managing polycystic ovary syndrome and endometriosis requires a holistic and personalised approach, as both conditions can significantly impact a woman’s quality of life and overall health.
For managing PCOS, lifestyle modifications are often the first line of defence. A balanced diet, regular exercise, and maintaining a healthy weight can significantly reduce symptoms and improve the condition. These changes are particularly effective in managing insulin resistance, a common aspect of PCOS. Medications may also be prescribed, such as hormonal birth control to regulate menstrual cycles or medication to improve insulin sensitivity. In some cases, fertility treatments might be necessary for those struggling with conception due to PCOS.
Endometriosis management often focuses on pain relief and controlling the progression of the condition. Pain management can include over-the-counter pain relievers, hormone therapy to reduce or eliminate periods, and in some cases, surgical options to remove endometrial tissue growth. Diet and exercise can also play a role, particularly in reducing inflammation. For fertility issues related to endometriosis, assisted reproductive technologies such as IVF are often considered.
Both conditions also benefit from complementary therapies. Practices like yoga, acupuncture, and mindfulness for women can help manage stress and pain. Support groups or counselling can be beneficial, providing emotional support and coping strategies.
Regular follow-ups with healthcare providers are essential for both PCOS and endometriosis. These appointments can help monitor the conditions, adjust treatments as necessary, and address any new symptoms or concerns. Remember, each individual’s experience with PCOS and endometriosis can be unique, so treatment plans should be tailored to meet personal health needs and lifestyles.