Managing the four phases of the menstrual cycle is a full-time job you never signed up for. Nonetheless, as a woman of reproductive age, maintaining a constant supply of period products, scheduling holidays around your bleed, and tracking dates when you’ll be ovulating are just a few of the tasks included on your invisible gender contract.
Understandably, missing your period for a month or two may feel like a massive relief. However, when you notice a missed period for three or more consecutive months, or experience irregular periods, these are signs that differ from what’s considered a normal menstrual cycle.
Missed or irregular periods fall under the medical condition of amenorrhea, and they can be a sign of more serious health conditions, like polycystic ovary syndrome (PCOS). So it’s important to track your menstrual periods from the day when periods start, and if they stop altogether. That way, you’re one step ahead when it’s time to find out what’s causing missed periods and how to overcome them.
What is amenorrhea?
Amenorrhea is the term used to describe an absence of menstrual bleeding, or missed periods in simple terms. We’re not talking about intentionally skipping your period using the pill. Amenorrhea is an unexplained disappearance of menses (the blood and matter expelled from the uterus during menstruation) that many women experience during their lifetime.
There are two types of amenorrhea: primary amenorrhea and secondary amenorrhea.
What’s the difference between primary and secondary amenorrhea?
Primary amenorrhea refers to young women who haven’t had their first menstrual period by the age of 15, or three years post-thelarche (that’s the term for the beginning of puberty when the secondary breasts are formed, amongst other things).
Secondary amenorrhea is characterised by an absence of regular menstruation for three months or longer, or irregular periods for six months or longer.
What are the symptoms of amenorrhea?
Aside from missing periods and menstrual irregularities, other symptoms of amenorrhea include:
Milky discharge from nipples
Hair loss
Headache
Vision changes
Excess body hair
Excess facial hair
Changes in breast size
Pelvic pain
Acne
What causes amenorrhea?
Amenorrhea is often a sign of another health problem rather than an individual condition, and it can occur for many reasons. The most common cause of amenorrhea is pregnancy. Once pregnancy has been ruled out via pregnancy test or a visit to the gyno, causes of amenorrhea depend on whether the amenorrhea is primary or secondary.
What causes primary amenorrhea?
The main causes of primary amenorrhea in young women are:
Delayed puberty
Chromosomal or genetic abnormalities
Certain chromosomal (relating to DNA) or genetic (relating to genes) abnormalities can cause the ovaries to stop functioning properly.
Examples include:
Turner syndrome, a condition caused by a partially or completely missing X chromosome
Mullerian agenesis, a birth defect characterised by a malformation of the genital tract
Androgen insensitivity syndrome, a condition characterised by high levels of testosterone
Issues with the hypothalamus or pituitary gland
Issues with the hypothalamus (a region of the brain that controls important bodily functions) and pituitary gland can cause a hormonal imbalance that prevents a first period from starting.
Eating disorders, excessive exercise, and extreme physical or psychological stress can also cause missed periods by preventing normal functioning of the hypothalamus or pituitary gland.
Hypothyroidism
A condition that decreases thyroid hormones responsible for functions associated with metabolism, puberty and the menstrual cycle.
What causes secondary amenorrhea?
The causes of secondary amenorrhea are:
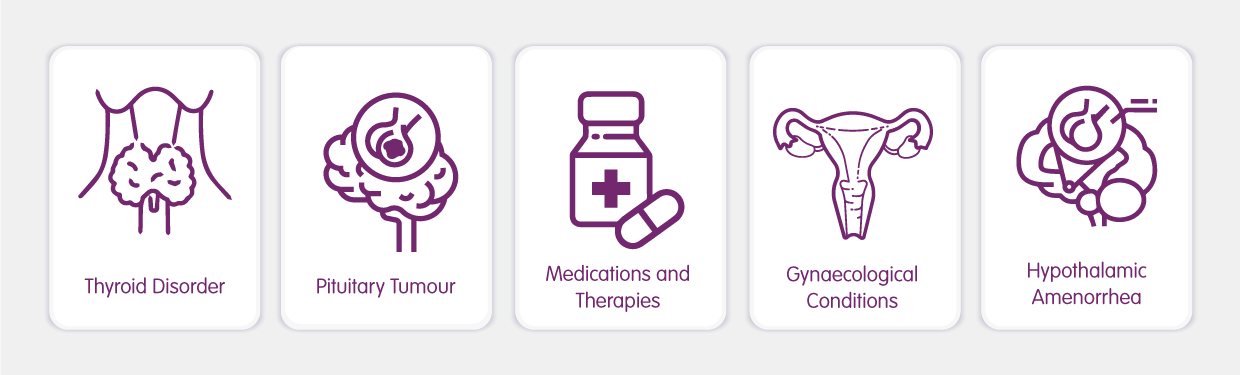
Thyroid disorders
A small butterfly-shaped gland at the base of the neck, the thyroid gland produces hormones that control metabolism and assist in puberty and menstruation. An overactive or underactive thyroid can trigger menstrual irregularities, including amenorrhea.
Pituitary tumours
Located in the brain, the pituitary gland controls hormone production and influences bodily functions linked to the female reproductive system and metabolism. Tumours on the pituitary gland can hinder the body’s hormonal regulation of menstruation.
Medications and therapies
Some birth control pills and intrauterine devices (IUDs) can cause amenorrhea.
Certain antidepressants and blood pressure medications can increase the levels of a hormone that prevents ovulation and the menstrual cycle from occurring.
Common cancer treatments of chemotherapy and radiation therapy can destroy estrogen-producing cells and eggs in the ovaries, leading to short-term amenorrhea.
The medical procedure referred to as a dilation and curettage (D&C) removes tissue from the uterus to manage heavy bleeding, clear the lining of the uterus post-miscarriage, or treat uterine fibroids. This procedure can cause uterine scarring that stops normal periods.
Gynaecological conditions
Gynaecological conditions that result in imbalanced hormones can cause secondary amenorrhea.
These include polycystic ovary syndrome (PCOS), a condition that occurs when a woman’s body overproduces androgens (the group of male hormones), and Fragile X-associated primary ovarian insufficiency (FXPOI), a condition in which a woman’s ovaries stop functioning prior to menopause.
Hypothalamic amenorrhea
Hypothalamic amenorrhea occurs when the hypothalamus (a gland in the brain) slows or stops releasing the hormone responsible for triggering the menstrual cycle, the gonadotropin-releasing hormone (GnRH).
Attributes of hypothalamic amenorrhea include low body weight, low body fat percentage, low caloric intake, intense exercise that burns more calories than those that are consumed through food, leptin deficiency, and emotional stress.
Diagnosis of amenorrhea
If your period has disappeared and you’re concerned you have amenorrhea, speak with your doctor who will be able to identify the cause of amenorrhea through a series of medical tests, including:
Pregnancy testing, involving either a blood or urine sample
Physical examination to check overall health and existing health conditions
Hormonal testing
Ultrasound of the reproductive system
Medical history, inclusive of gynaecological history and contraceptive usage
How do you treat amenorrhea?
Treatment for amenorrhea varies depending on the underlying cause and individual health status. Lifestyle factors incorporating diet, exercise, and stress management can help, particularly if missed periods are caused by weight loss or malnutrition. Certain hormonal medications and oral contraceptives can help trigger a period by administering hormones. If amenorrhea occurred as the result of an eating disorder, therapy may prove beneficial.
In rare instances, surgery may be required to correct chromosomal or genetic defects, remove a pituitary tumour, or remove uterine scar tissue.
The best treatment plan is the one personalised by your trusted healthcare professional based on your unique situation.
What can you do to prevent amenorrhea?
Amenorrhea can result from a wide range of lifestyle factors, so it isn’t 100-percent preventable. To give yourself the best chance of preventing amenorrhea, aim to:
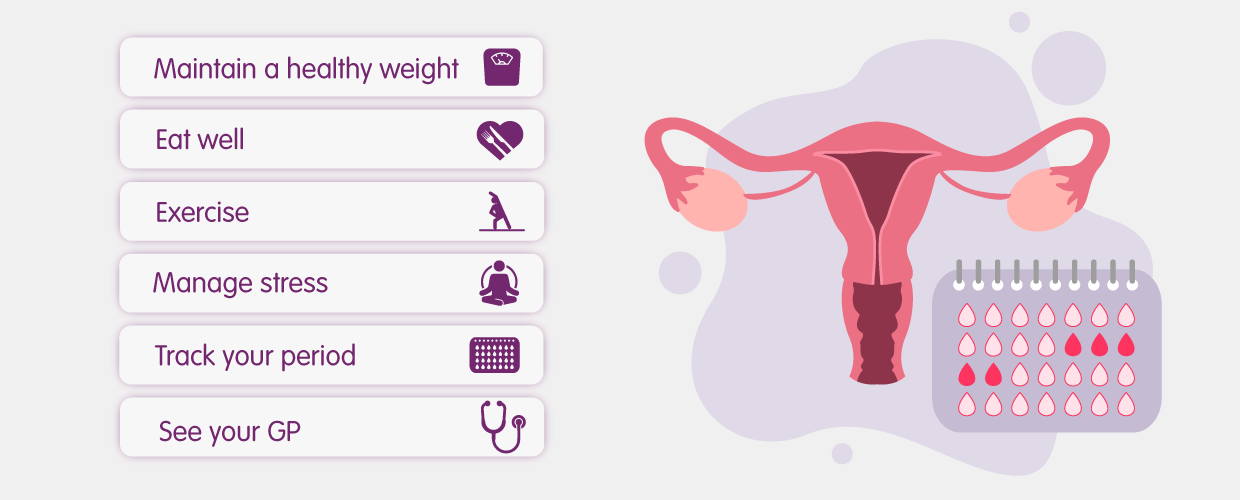
Maintain a healthy weight
Eat a well-balanced diet
Exercise regularly
Manage stress (tip: learning how to practice mindfulness may help)
Use the best period tracking apps to monitor changes or abnormalities that occur in your cycle
See your doctor when symptoms first arise
Can you get pregnant if you have amenorrhea?
We’re here to help!
If missed periods are causing worry in your life, chat with one of our Aussie doctors to see what options are available for you.