Possible causes of chronic pelvic pain
If you’re a woman who’s ever experienced pain or discomfort in the lower abdomen, between your belly button and vulva, it could have been pelvic pain. And, yes, we agree that persistent pelvic pain easily takes a podium place on the list of discomforts experienced by women.
Due to the important female reproductive organs housed within the pelvis, pelvic pain can be experienced in many different ways depending on the underlying cause of the pain. Some women deal with sharp pain in their pelvic region specifically during their menstrual cycle, while others live with severe chronic pain that lingers throughout all four phases of the menstrual cycle.
While the causes of pelvic pain vary, from menstrual cramps and ovulation to food intolerances and gastrointestinal issues, the discomfort can often be accompanied by severe pain that significantly affects one’s quality of life and can be a sign of a more serious health condition.
Since we’re all about sharing essential women’s health information, let’s look at some of the most common causes of pelvic pain in women. But remember, it’s always important to have pelvic pain professionally diagnosed by a doctor to understand the cause and correct medical treatment.
So, what does pelvic pain feel like?
Pelvic pain can feel like a dull ache or a stabbing, sharp pain. It can be constant, or it can sporadically appear and disappear. Pelvic pain can also feel like pressure in the pelvis or like something is pulling or stretching in the pelvis. Some women describe pelvic pain as feeling heavy in their lower abdomen or pelvis.
Pelvic pain can be a sign of many different conditions, including endometriosis, pelvic inflammatory disease, ovarian cysts, and more.
Possible causes of pelvic pain in women
Endometriosis
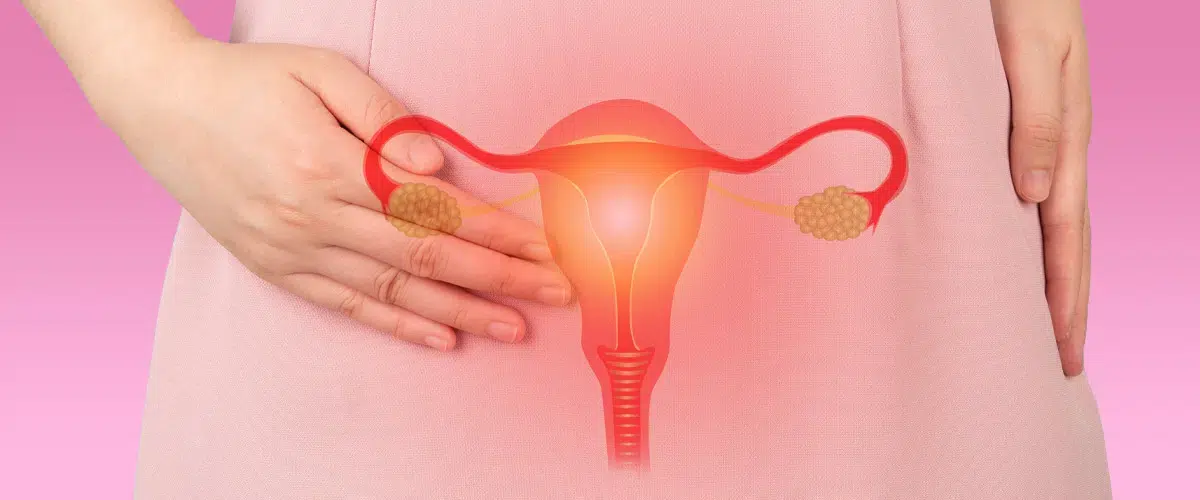
One of the leading causes of pelvic pain and fertility problems in women, endometriosis is a chronic, estrogen-dependent condition in which the endometrium (the tissue that lines the uterus) grows outside of the uterus.
Endometriosis most commonly affects women of reproductive age and features common symptoms of pelvic pain, painful periods, and infertility. There is no cure for endometriosis; however, early diagnosis and treatment can help to reduce the impact of the condition.
Premenstrual syndrome (PMS) and menstrual cramps
One common health condition that can cause pelvic pain is premenstrual syndrome (PMS). The condition of period pain is caused by hormonal changes that occur during the menstrual cycle, and symptoms can include pelvic pain, bloating, breast tenderness, headaches, and mood swings.
Then we have menstrual cramps – a super common cause of pelvic muscle pain brought on when the uterus contracts to expel menstrual blood and tissue during the menstrual phase of the menstrual cycle.
If you frequently experience pelvic pain during ‘that time of the month’, it is important to see your doctor to determine the cause. Treatment will depend on the underlying condition that causes pelvic pain. In some cases, over-the-counter pain medications may be enough to relieve the painful symptoms. Otherwise, your doctor may prescribe stronger medication for severe pain.
Pelvic congestion syndrome (PCS)
Pelvic congestion syndrome (PCS) is a condition where the pelvic blood vessels become dilated and congested. This can cause pain in the pelvis, lower back, and legs. Pelvic congestion syndrome is most often seen in women of childbearing age; however, it can occur at any age.
The exact cause of pelvic congestion syndrome is unknown, yet it is thought to be related to hormonal changes, chronic inflammation, or abnormalities in the pelvic veins or lymphatic system.
Treatment for pelvic congestion syndrome typically involves medications to relieve pain and swollen blood vessels. Surgery may also be necessary to remove damaged tissue or blockages in the vessels. In some cases, treatment may also involve lifestyle changes such as losing weight, exercising, and avoiding tight clothing.
Pelvic congestion syndrome can be a chronic and debilitating condition. However, with proper medical care, most women can manage their symptoms and live relatively normal lives.
Kidney Stones
Another big hitter when it comes to the culprits of pelvic pain is kidney stones. Ranging in size from a tiny grain of sand to a large pebble, kidney stones cause excruciating pain as they make their way through the urinary tract and into the toilet bowel. There are several different types of kidney stones, but the most common type is made up of calcium oxalate.
Treatment for kidney stones and pelvic pain often depends on the underlying cause. If an infection is to blame, antibiotics may be prescribed. If endometriosis is the cause, hormone therapy or surgery may be recommended. Pain relief medication, such as over-the-counter ibuprofen, can also help to ease the discomfort associated with both kidney stones and pelvic pain.

Urinary Tract Infections
Urinary tract infections (UTIs) are another cause of pelvic pain. UTIs are most often caused by unwanted bacteria that enter the urinary tract through the urethra and multiply in the bladder.
Symptoms of a UTI include a burning sensation when peeing or having sex, cloudy or bloody urine, and pelvic pain. Treatment for a UTI typically includes antibiotics.
Irritable bowel syndrome
Irritable bowel syndrome (IBS) is a condition that can cause a variety of symptoms, including abdominal pain, bloating, gas, diarrhoea, and constipation. While the exact cause of IBS is unknown, it is thought to be related to an imbalance in the nervous system that controls the digestive system.
Pelvic pain is a common symptom of IBS and can be caused by a variety of factors, including muscle spasms in the pelvis, inflammation of the intestines, or constipation. Treatment for IBS typically includes lifestyle changes, such as diet and stress reduction, and medication. In some cases, surgery may be necessary to relieve severe symptoms.
Pelvic floor dysfunction
In some cases, pelvic pain may be caused by a condition known as pelvic floor dysfunction. This is a disorder of the pelvic muscles and tissues that support the pelvis.
Symptoms of pelvic floor dysfunction can include pain during urination or bowel movements, difficulty urinating or having a bowel movement, and pain during sex. Treatment for pelvic floor dysfunction typically includes physical therapy.
Ovarian Cysts
Ovarian cysts are fluid-filled sacs that can form on the ovaries, and they’re usually harmless, but a cause of pelvic pain nonetheless. Ovarian cysts can cause pain, discomfort, and a variety of other symptoms, including breast tenderness, irregular periods, and bloating in women. In some cases, they can also lead to more serious problems like rupture or ovarian torsion (twisting of the ovary).
There are two types of ovarian cysts: functional and pathological. Functional cysts are the most common and usually form during ovulation. Pathological cysts are less common and can be caused by several different things, including endometriosis, infection, or tumours.
If you’re experiencing any symptoms of an ovarian cyst, it’s important to see your doctor. They can perform a physical exam and order tests to confirm the diagnosis. Treatment will depend on the type and severity of your symptoms but may include over-the-counter pain medication, birth control pills, or surgery.
Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease (PID) is a general term used to describe acute pelvic pain and infection of the female reproductive organs (psst – have you checked out our guide to female anatomy yet?).
PID typically occurs when bacteria from the vagina or cervix travel up into the uterus, fallopian tubes, or ovaries. The most common cause of PID is a sexually transmitted infection (STI), such as chlamydia or gonorrhoea. However, other infections such as pelvic tuberculosis can also cause PID.
Symptoms of PID can vary from mild to severe and may include abnormal vaginal discharge that may have an unpleasant odour, abnormal vaginal bleeding, such as bleeding between periods or after intercourse, pain in the lower abdomen, pelvis, or both, fever, chills, nausea, vomiting, loss of appetite, painful urination, and fatigue.
If you think you may have PID, it is important to see a doctor as soon as possible. If left untreated, PID can lead to serious complications such as infertility, ectopic pregnancy, and chronic pelvic pain. Treatment for PID usually involves a course of antibiotics. Surgery may also be necessary in some cases.

Sexually transmitted infections (STIs)
There are several sexually transmitted infections that can cause pelvic pain. These include chlamydia, gonorrhoea, and trichomoniasis. Pelvic pain can also be caused by other STIs, such as syphilis, HIV, and HPV.
While most STIs can be treated with medication, some, like HIV and HPV, have no cure. In these cases, the focus is on managing the symptoms and preventing the disease from spreading (hence the importance of having regular cervical screenings). If you think you may have an STI, see your doctor so that you can get tested and start treatment if necessary.
Interstitial Cystitis (IC)
Interstitial cystitis (IC), also known as painful bladder syndrome, is a chronic condition that causes pain and inflammation in the bladder. Symptoms of IC can include pelvic pain, urinary frequency and urgency, and sexual dysfunction.
The exact cause of IC is unknown, but it is believed to be a multi-factorial disease, potentially caused by a combination of factors, including urinary tract infection, immune system dysfunction, and changes in the structure of the bladder.
There are a variety of treatments available for IC, depending on the severity of the symptoms. Some treatments aim to relieve pain, while others focus on reducing urinary frequency and urgency. Treatment options include medication, dietary changes, physical therapy, and surgery.
Interstitial cystitis is a chronic condition that requires long-term pain management. There is no cure for IC, but treatment can help to improve symptoms and quality of life.
Uterine Fibroids
Uterine fibroids are common non-cancerous growths that occur in the uterus. They are made up of smooth muscle and connective tissue and can vary in size. Fibroids can grow on the outside of the uterus, in the uterine cavity, or they can be attached to the uterine wall by a stalk.
Pelvic pain is a common symptom of uterine fibroids, with pain varying in intensity and being sharp, dull, or aching. It can be intermittent or constant and may worsen with certain activities such as intercourse or urination.
Pelvic pain often occurs as a result of the pressure that fibroids place on surrounding organs or from the stretching of the uterine wall as the fibroids grow. In some cases, pelvic pain may also be caused by an infection or inflammation of the fibroids.
In addition to pelvic pain, uterine fibroids can also cause several other symptoms, including heavy or prolonged menstrual bleeding, anaemia (low red blood cell count) as a result of heavy bleeding, menstrual pain, pelvic pressure or fullness, urinary frequency or urgency, constipation, backaches or leg pain, fertility problems, and pregnancy complications, such as miscarriage, preterm labour, or low birth weight infants.
Pelvic Organ Prolapse
There are several different types of pelvic organ prolapse, and they can vary in severity. The most common type is uterine prolapse, which occurs when the uterus drops down into the vagina. This can cause pain and discomfort and may make it difficult to have sexual intercourse.
Pelvic organ prolapse is usually caused by weak pelvic floor muscles. These muscles support the organs in the pelvis, and when they are weakened, they can no longer hold the organs in place. Pelvic organ prolapse can also be caused by pregnancy and childbirth, which can stretch and weaken the pelvic floor muscles.
Pelvic organ prolapse is usually treated with pelvic floor exercises and surgery. Surgery is usually only recommended if the prolapse is severe or if other treatments have failed.
Painful Sex
Sexual intercourse can cause pelvic pain in some women. This is usually due to the pressure of penetration, which can irritate the sensitive tissues in the pelvis. In some cases, this can also be caused by an infection or other medical condition.
If you’re experiencing persistent pain in the pelvic area during sex, talk to your doctor to find out the potential causes. Also, check out 6 reasons why your vagina may be sore after sex.
Scar tissue
Scar tissue can cause pelvic pain in women. The pain may be caused by the scar tissue itself, or by the way it affects surrounding organs. In women, the pain may be caused by scar tissue that has adhered to the ovaries, fallopian tubes, or uterus. Pelvic pain caused by scar tissue is often worse during menstruation or sexual activity.
Treatment for pelvic pain caused by scar tissue depends on the underlying cause. If the pain is due to compression of nerves, treatment may involve surgery to release the pressure on the nerves. If the pain is caused by scar tissue adhering to organs, treatment may involve surgery to remove the scar tissue. In some cases, both types of surgery may be necessary.
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilised egg implants outside of the uterus, most often in the fallopian tubes. This can cause the tube to rupture, leading to severe bleeding.
Ectopic pregnancy and pelvic pain often go hand-in-hand. Pelvic pain is a common symptom of ectopic pregnancy, occurring in up to 90% of cases. The pain is usually sharp and crampy, and can radiate to the shoulder or neck. It may be worse with movement, coughing, or urinating.
Ectopic pregnancy is a medical emergency and requires immediate treatment.
When should you worry about pelvic pain?
Pelvic pain is a common symptom of many conditions involving the female reproductive system. Some causes of pelvic pain are benign conditions, such as menstrual cramps or ovulation, while others may be more serious, such as endometriosis or uterine fibroids.
If you’re experiencing pelvic pain, it’s important to pay attention to other symptoms you may be experiencing along with the pain. For example, if you’re also experiencing fever, vaginal discharge, or excessive bleeding, this could be a sign of a more serious condition.
If you’re unsure about what’s causing your pelvic pain, or if the pain is severe, it’s always best to see your doctor for a medical assessment. Your doctor can determine the cause of your pain and recommend the appropriate treatment.
How is pelvic pain diagnosed?
There are a few different ways that doctors can diagnose pelvic pain beyond the diagnostic tools of blood and urine tests.
One way is to do a pelvic exam. During a pelvic exam, the doctor will feel the pelvis and abdomen for any tenderness or swelling. They may also order an ultrasound or MRI to take a better look at the pelvis and abdomen.
Another way to diagnose pelvic pain is through a laparoscopy. During a laparoscopy, the doctor will make a small incision in the abdomen and insert a small camera. This will allow them to take a closer look at the pelvic organs and see if there is any tissue that looks abnormal.