Let’s talk about PCOS. Four simple letters that define a complex hormonal condition known as polycystic ovary syndrome that affects 6 – 18% of women of reproductive age worldwide¹. The thing with PCOS is that no two cases of PCOS are identical. Each person experiences a unique set of symptoms, making PCOS a challenging condition to (1) identify and (2) diagnose.
Since early diagnosis is vital to ensuring proper management of symptoms and risk reduction of long-term health conditions, such as Type-2 Diabetes (a metabolic syndrome) and cardiovascular disease, the best weapon in any female arsenal is knowing everything about PCOS. From PCOS symptoms to causes and treatment options, it’s time to familiarise yourself with one of the most misunderstood women’s health conditions.
What is polycystic ovary syndrome (PCOS)?
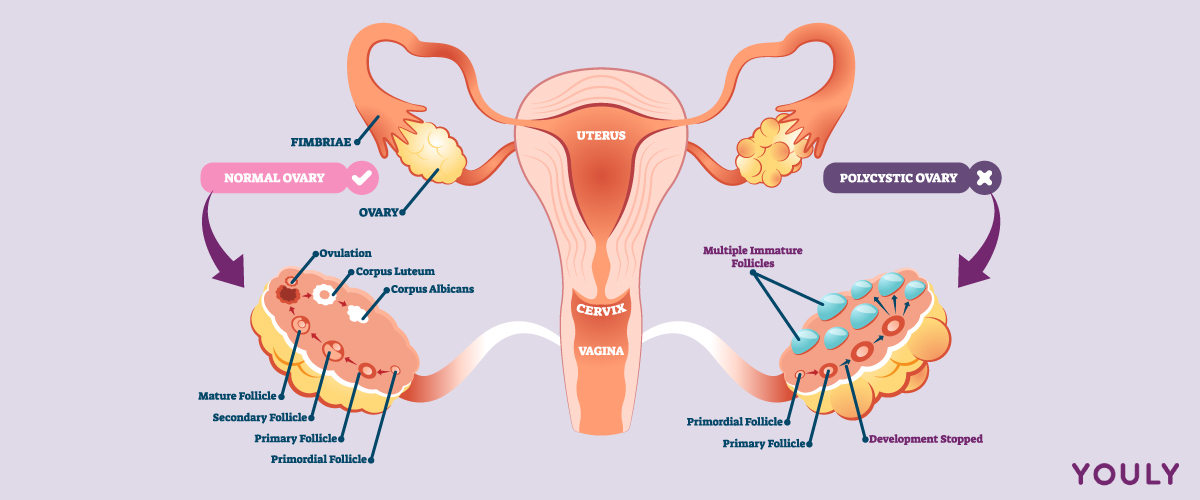
Polycystic ovary syndrome is a disorder of the female reproductive system. Women with PCOS tend to produce an abnormally high amount of male sex hormones called androgens. In addition to the overproduction of male hormones, PCOS correlates with higher insulin levels, the hormone responsible for controlling how food converts into energy. Higher-than-normal levels of androgens can impact reproductive health and the menstrual cycle, sometimes preventing ovulation.
Despite the term ‘polycystic’ translating to ‘many cysts’, cysts aren’t always present in women with PCOS. When they exist, they aren’t typical cysts but small follicles containing an undeveloped egg that never matured.
PCOS risk factors
PCOS affects many women; however, the prominent risk factor for PCOS is genetics. A woman sits at a higher risk for PCOS if she is genetically predisposed to the condition, meaning she has other female family members with PCOS, irregular periods, or diabetes.
According to Jean Hailes;
“Women with PCOS are 50% more likely to have a mother, aunt, or sister with PCOS, and the condition is more common in women of Asian, Aboriginal, Torres Strait Islander and African backgrounds”.
What are the symptoms of PCOS?
Women with PCOS may present with a wide range of symptoms; the most common PCOS symptoms being cysts on the ovaries, oligomenorrhoea (irregular menstrual cycles), hirsutism (excessive facial or body hair growth), acne, and weight gain.
Women with PCOS may also experience other symptoms of:
- Amenorrhea (wait! What is amenorrhea?)
- Darkened or excess skin (skin tags) on the neck or armpits
- Thickened skin around the neck, armpits, or breasts (a sign of insulin resistance and high blood pressure)
- Thinning hair or scalp hair loss
- Reduced fertility (due to absent or infrequent ovulation)
- Weight gain
- Sleep apnoea
- Mental health conditions, like anxiety and depression
What causes PCOS?
What causes PCOS? That’s the mystery question.
The exact cause of PCOS is unknown. There is a hereditary factor and hormonal dysfunction resulting from several follicles failing to mature and release eggs, instead dying on the surface of the ovaries. Some experts also claim that the principal underlying disorder is insulin resistance, where the body doesn’t use insulin correctly, and hyperinsulinemia, where abnormally high insulin levels exist.
How is polycystic ovary syndrome (PCOS) diagnosed?
Up to 70% of women with PCOS remain undiagnosed². As well as presenting with unique and wide-ranging symptoms, according to Australian-led PCOS guidelines published in the Medical Journal of Australia, obtaining a timely PCOS diagnosis is challenging for women, with many experiencing delays with multiple doctors involved.
The journey to PCOS diagnosis is typically long, with one-third or more of women reporting >2 years (33.6%) and visiting ≥3 health professionals (47.1%) before receiving a formal diagnosis³.
A PCOS diagnosis requires two out of the following three criteria:
- Absent or irregular periods
- High androgen levels in the blood, OR symptoms of acne and excessive hair growth on the face or body
- An ultrasound showing partially developed eggs that look like dark circles on the ovaries (20 or more cysts on either ovary)
After two out of the three criteria above have been identified, medical history, examination, blood testing, and ultrasounds are used to diagnose PCOS.
Medical examination
A GP will review an individual’s medical history and perform a pelvic exam and a physical exam to assess symptoms, weight, and body mass index (BMI).
Blood tests
Blood tests assess blood glucose levels and hormone levels, such as androgens (male hormones) in the body. They may also be used to determine the levels of other reproductive hormones, such as oestradiol (oestrogen), follicle-stimulating hormone (FSH), and luteinizing hormone (LH), as these can impact period regularity.
Blood tests also rule out other health conditions with symptoms similar to PCOS by measuring the levels of prolactin (a hormone released by the pituitary gland that stimulates breast development and milk production in women), thyroid-stimulating hormone (TSH), and hormones related to adrenal function.
Ultrasound
An ultrasound of the reproductive organs can provide a snapshot of what’s happening with the uterus, ovaries, and pelvis. Of particular importance, an ultrasound can give evidence of cysts on the ovaries, whether an ovary is enlarged, and whether the lining of the womb (endometrium) is thickened, which is a common risk factor for uterine cancer.
Learn five different gynaecological cancers you shouldn’t ignore.
Transvaginal ultrasound
A transvaginal ultrasound is a painless test that uses a pen-shaped probe with an ultrasound sensor on the end to examine the vagina, providing a clearer image than an abdominal ultrasound. A transvaginal ultrasound is performed only on sexually active women. Otherwise, an abdominal ultrasound will be performed.
Abdominal ultrasound
An abdominal ultrasound provides images of the ovaries from outside the stomach wall.
Other diagnostic tests
Since PCOS is a health condition linked with insulin resistance and being overweight, it’s essential to assess the risk of developing heart disease and diabetes with:
- Cholesterol blood tests
- Blood pressure tests
- Glucose metabolism/tolerance blood tests
PCOS-related health issues
Weight gain
Many women with PCOS experience difficulty managing their weight, with increased weight gain causing higher levels of androgens and insulin, which can worsen symptoms⁴.
Psychological issues
Women with PCOS are at an increased risk of experiencing mental health problems like anxiety and depression⁵. It is not clear why this is the case; however, it may be due to hormonal imbalance and having to deal with the frustrating symptoms of PCOS.
Fertility issues
Hormone levels, irregular or missed periods, weight gain, and an unhealthy lifestyle can make it difficult for women with PCOS to get pregnant.
Other health issues linked to PCOS
There is a heightened risk of women with PCOS developing several other health conditions, such as prediabetes, type-2 diabetes, gestational diabetes, and cardiovascular disease⁶. These risks can be lowered with a healthy lifestyle, incorporating regular physical activity and a healthy diet for improved weight management.
How is PCOS treated?
Unfortunately, there is no cure for polycystic ovarian syndrome; it is a chronic disorder that requires long-term management to reduce the risk of developing long-term health problems. Depending on the present symptoms, PCOS can be managed through various lifestyle modifications and medical treatments.
Weight management
Maintaining a healthy weight can help treat PCOS by regulating hormone production, improving mood, and managing symptoms of facial and body hair growth, scalp hair loss, and acne. It can also reduce the risk of developing type-2 diabetes and cardiovascular disease by causing a positive effect on insulin levels⁷⁻⁹.
Ways to maintain a healthy weight include:
- Staying active
- Eating a healthy diet
- Losing weight if overweight
- Gaining weight if low body weight is causing irregular menstrual periods or missed periods
For a plan to lose weight, gain weight, or form sustainable healthy lifestyle habits, always consult your healthcare professional for the best advice for your situation.
Medical treatments
Hormonal birth control, such as the oral contraceptive pill, can help regulate the menstrual cycle, reduce excess hair growth and acne, and prevent the womb’s lining from excessive thickening. Birth control pills and the diabetes drug metformin can also help manage insulin resistance.
Further to this, medications that block hormones can help reduce excess hair growth and scalp hair loss. Insulin-sensitising medications can help regulate menstrual cycles, improve ovulation and fertility, and assist with weight loss. Fertility medication can also help reduce potential pregnancy complications.
Cosmetic treatments
Cosmetic treatments, such as laser hair removal, may help many women with PCOS to feel better about their appearance if excess hair growth is a symptom.
For the best course of treatment to manage PCOS and improve PCOS symptoms, it’s always best to consult with a trusted doctor or medical practitioner.
For a PCOS diagnosis, always consult with your doctor. For online birth control and women’s health needs, visit Youly.
Sources
- Deswal, Ritu et al. “The Prevalence of Polycystic Ovary Syndrome: A Brief Systematic Review.” Journal of human reproductive sciences vol. 13,4 (2020): 261-271. doi:10.4103/jhrs.JHRS_95_18
- Polycystic Ovary Syndrome. Royal Australian College of General Practitioners (RACGP). October 2012. https://www.racgp.org.au/afp/2012/october/polycystic-ovary-syndrome/
- Palomba, S., Orio Jr, F., Falbo, A., Russo, T., Zullo, F., Russo, I. “Diagnostic delay in polycystic ovary syndrome: an overview.” Hum Reprod Update. 2009 Sep-Oct;15(5):567-76.
- Moran, L.J., Misso, M.L., Wild, R.A., Norman, R.J. “Impaired glucose tolerance, type 2 diabetes and metabolic surgery in polycystic ovary syndrome.” Nat Rev Endocrinol. 2016 Mar;12(3):139-53.
- Williams, M.J., Harris, M.A., Phillips, K.A., Wilcock, A., Shields, B. “The prevalence of depression and anxiety in women with polycystic ovary syndrome: a systematic review.” Hum Reprod Update. 2014 Nov-Dec;20(6):794-808.
- Dumesic, D.A., Lobo, R.A. “Polycystic ovary syndrome: etiology, pathogenesis and diagnosis.” Nat Rev Endocrinol. 2011 Mar;7(3):219-31.
- Bochicchio, R., Eisermann, K., Testa, G., Ferrari, F., Restelli, A., Giallonardo, A. et al. “Weight loss in overweight-obese women with polycystic ovary syndrome: effects on body composition, androgens, insulin sensitivity, and subcutaneous fat distribution.” Eur J Endocrinol. 2011 Oct;165(4):667-74.
- Nasiri, N., Azarbarzin, A., Roshanfekr, H., Mirmiran, P., Azizi, F. “The effect of lifestyle modification on anthropometric, metabolic, hormonal and clinical characteristics in women with polycystic ovary syndrome: a randomized controlled trial.” J Endocrinol Invest. 2017 Sep;40(9):901-910.
- Morin-Papunen, L.C., Vauhkonen, I., Koivunen, R., Martikainen, H., Tapanainen, J.S., Ruokonen, A. “Lifestyle changes in the management of polycystic ovary syndrome.” Best Pract Res Clin Obstet Gynaecol. 2013 Aug;27(4):423-37.