Including: how to self-collect for your cervical screening test.
If we told you cervical cancer was largely preventable, we bet you’d dive into asking how.
The answer is simple: with early detection through regular cervical screening tests, cervical cancers can be prevented, or treatment for pre-existing cancers can be sought early to significantly improve cervical cancer survival.
The National Cervical Screening Program
In 1991, the Australian government introduced the National Cervical Screening Program; a pivotal program responsible for halving cervical cancer incidence and mortality rates in Australia.
In 2007, further changes to the National Cervical Screening Program saw the introduction of a vaccine against specific strains of the human papillomavirus (HPV), the virus responsible for causing almost all cervical cancers in women and people with a cervix.
The updated program – including both the cervical screening test and the HPV vaccine – replaced the pap test and has provided protection against cervical cancer while reducing cervical cancer rates and deaths by at least 20% in Australia.
What is HPV?
HPV is a super common virus that is transmitted sexually or via skin-to-skin contact. There are over 100 strains of HPV, and 4 out of 5 people carry at least one type of HPV virus at some stage of their lives¹.
HPV infection can be asymptomatic, or HPV infection can cause skin or mucous membrane growths (warts) and sometimes different types of cancer. Most HPV infections don’t lead to cancer, however, some types of genital HPV infection can cause cancer of the cervix – the lower part of the uterus that connects to the vagina.
Find out more about the cervix (including what does a cervix look like?).
There is no treatment for an HPV infection, and often the body’s immune system defeats an infection before it has a chance to form visible warts.
The HPV vaccine
Since early cervical cancers don’t cause symptoms, and they can take 20 years or more to develop after an HPV infection, getting the HPV vaccine is the best protection against the strains of HPV most likely to cause genital warts or cervical cancer.
Additionally, it’s recommended that women and people with a cervix have regular cervical screening tests that can be used for detecting HPV and precancerous cell changes in the cervix that may potentially lead to cancer.
What is the cervical screening test?
Replacing the Pap tests in 2017, the cervical screening test is the best protection against cervical cancer, making cervical cancer one of the most preventable cancers in existence. The cervical screening test works to prevent cervical cancer by detecting cancer-causing strains of HPV and abnormal cells in a sample of cells collected from the cervix.
There are two safe and effective methods to collect a test sample in Australia: a healthcare provider sample collection, or a newly introduced self-collection.
Healthcare provider sample collection
If you choose to have a healthcare provider perform your cervical screening tests, you’ll need to visit your general practice where specially trained health professionals can perform a cervical screening test using a speculum and a small brush (kind of like a cotton swab) to collect a sample from your cervix.
Self-collection
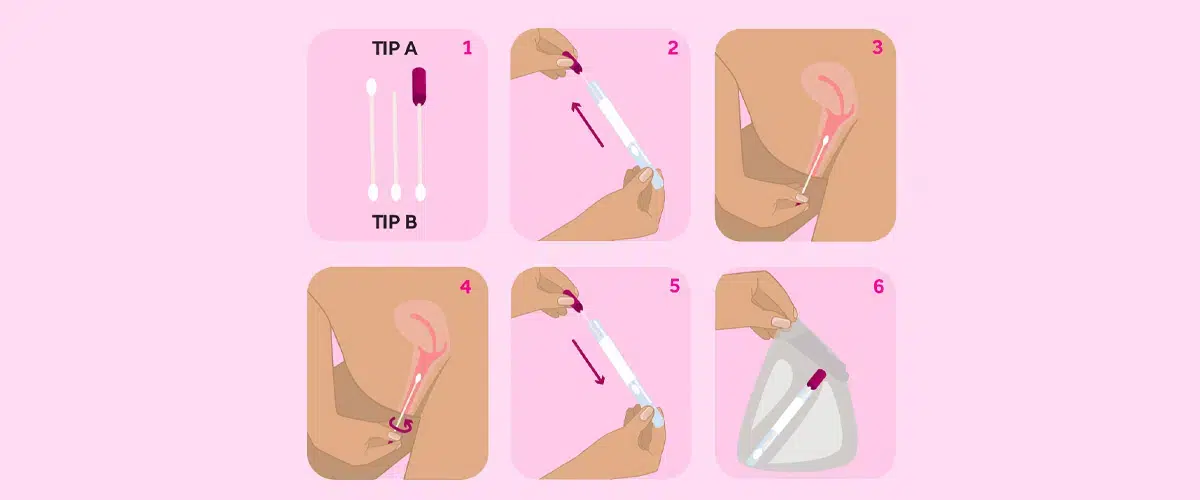
From the 1st July, 2022, self collected vaginal sample became a viable option for Australian women hoping to complete a regular cervical screening.
To perform a self collection, you will still need to visit your general practice. Your doctor or nurse will provide you with a self collection swab and instructions on how to collect a sample of cells from your vagina. They’ll then escort you to a private space to collect your sample yourself.
Self collection is equally effective at detecting HPV, however it is not a suitable option if you are or have been experiencing health symptoms, such as abnormal vaginal bleeding, pain, or discharge.
Is a cervical cancer screening painful?
A cervical cancer screening shouldn’t be painful, however a minor discomfort may be experienced. If you feel uncomfortable or are worried about pain, talk to your doctor about ways to make your cervical screening more comfortable for you.
Who needs the cervical screening test?
Current Australian guidelines state that you are eligible for a cervical screening if you are aged 25 to 74, have a cervix, and have ever been sexually active. There’s no need for women to have a cervical cancer screening any earlier – it’s completely safe to wait until the age of 25 to have the first cervical screening test.
If the last cervical screening test you had was a pap test, you can introduce the new cervical screening test 2 years after your last Pap test. Then, plan a cervical screening test every two years, unless abnormal symptoms present (e.g. unusual bleeding).
Getting your cervical screening test results
When your results are ready, they will be sent to the clinic where you had your test, or to a clinic that your nominate. Your results will also become available on the National Cancer Screening Register.
The National Cancer Screening Register enables a digital record for each person in Australia participating in cervical cancer screening. The register provides better access to quality health information – another one of the ways Aussie women can take control of their health.
What do my results mean?
Your healthcare provider will talk to you about your Cervical Screening Test results. Based on your results, your healthcare provider may recommend that you:
- return to screen in 5 years
- return to have a secondary sample collected by your healthcare provider
- repeat the test in 12 months
- repeat the cervical screening test due to unsatisfactory test result
- see a specialist.

Return to screen in 5 years
If your doctor asks you to return for a sample in five years, this is great news! Your screening results show that you do not have a HPV infection. The National Screening Register will sent you a reminder closer to the date of your next screening.
Return for another sample collected by your healthcare provider
If you self collected your sample and your results identify the early stages of a potential HPV infection, you may need to return to your doctor to confirm if the infection has caused cervical cell changes that require further testing.
A self collection does not test for cervical cells, hence the need to return to your doctor who will collect a sample from your cervix.
Repeat the test in 12 months
If your doctor requests a follow up screening in 12 months, you likely have a HPV infection that will be cleared by the body within the next 12 months. You’ll need the follow up test to confirm the infection has cleared during that time, and you are safe to return to screening every 5 years.
Repeat the Cervical Screening Test due to unsatisfactory test result
An unsatisfactory result occurs when your sample cannot be analysed correctly by the laboratory for whatever reason. This doesn’t mean there is something wrong, simply that you need to re-test within the next 6-12 weeks.
Referral to a specialist
If your doctor refers you to a specialist following your cervical screening, this means that your results show you have a type of HPV infection that needs further investigation by a specialist.
It doesn’t mean you have developed cervical cancer. You may need a follow up test, such as a colonoscopy.
Just like cervical cancer screenings are a great way for women to take control of their health, our digital healthcare platform is the easiest way to get your prescriptions delivered to your door for the ultimate in hassle-free healthcare!