Eczema and psoriasis are two of the most common skin conditions affecting women. Both conditions can cause patches of dry, irritated and itchy skin. And both conditions are chronic, meaning they may hang around for life. However, eczema and psoriasis have distinct differences in symptoms, causes, and treatments.
So if the difference between eczema and psoriasis is an itch you need to scratch, we’re here to help you with the key symptoms, causes, risk factors, and treatments of eczema and psoriasis.
What is eczema?
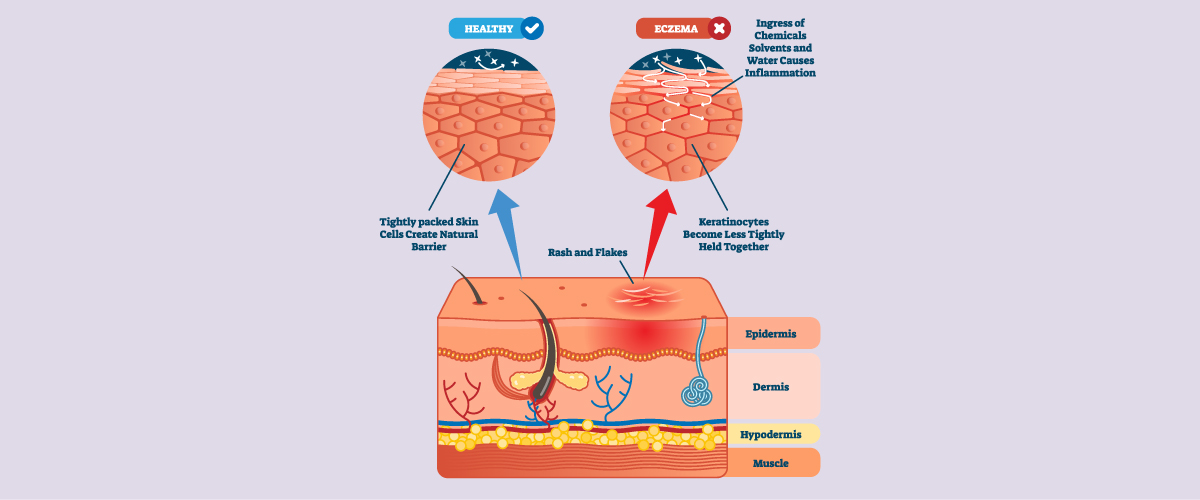
Eczema, also known as atopic dermatitis, is a chronic skin condition that causes the skin to become itchy, red, and inflamed. It is a common condition that can affect people of all ages, but it is most commonly diagnosed in children.
Eczema typically occurs on the face, hands, and feet; however, it can appear anywhere on the body. Symptoms of eczema include dry, scaly skin, itching, redness, and raw, sensitive skin due to scratching.
In some cases, eczema can also cause small, fluid-filled blisters on the skin.
According to the Australasian Society of Clinical Immunology and Allergy (ASCIA), eczema affects around 20% of children and 10% of adults in Australia¹.
Types of eczema
There are several types of eczema, each with its symptoms and characteristics. The most common types include:
Atopic dermatitis (atopic eczema)
The most common type of eczema, atopic dermatitis, is characterised by itching, redness, dryness, and the formation of eczema lesions, which can be weepy or crusted. Atopic dermatitis is often associated with allergies and asthma.
Contact dermatitis
A type of eczema caused by direct contact with an irritant or allergen, such as a chemical, soap, or fabric. Symptoms include redness, itching, and a rash at the contact site.
Seborrheic dermatitis
Also known as dandruff, seborrheic dermatitis is characterised by greasy, yellowish scales on the scalp, face, and other oily areas of the body. It is more common in adults than children.
Dyshidrotic eczema
This type of eczema is characterised by small, itchy blisters on the hands and feet. It is more common in women than men and is often associated with stress.
Nummular eczema
A type of eczema characterised by coin-shaped, itchy, scaly patches on the skin, usually on the legs, arms, and trunk. It is more common in older adults and is often associated with dry skin.
Stasis dermatitis
This type of eczema is characterised by red, itchy, and scaly patches on the lower legs, usually in people with varicose veins or other circulatory issues.
What is psoriasis?
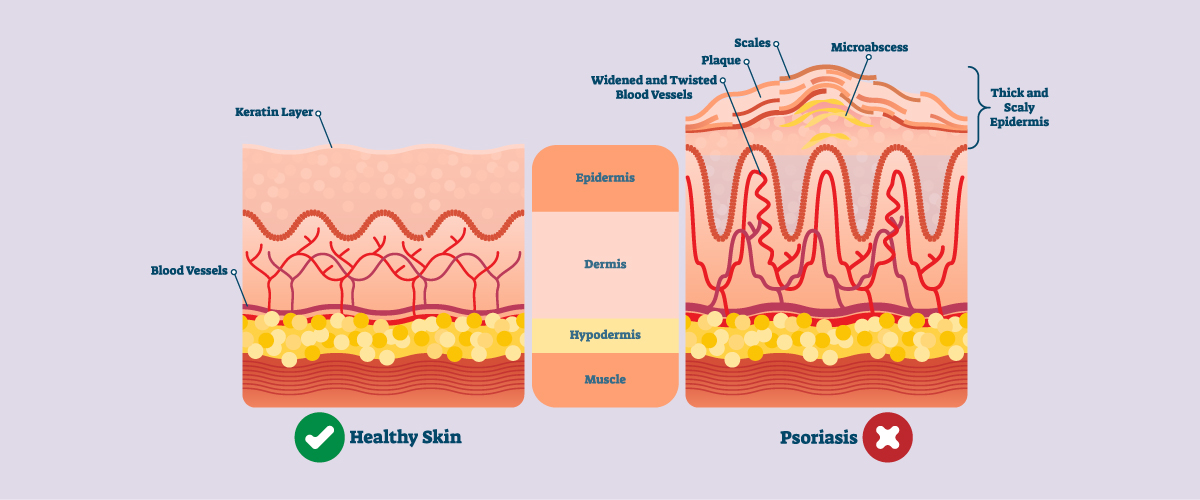
Psoriasis is a chronic autoimmune skin condition that causes cells to build up rapidly on the skin’s surface. The extra skin cells form scales and red patches that are sometimes itchy and painful.
Psoriasis typically affects the skin on the elbows, knees, scalp, lower back, face, palms and soles of feet; however, it can also affect nails, genitals, and the mouth. Psoriasis symptoms can vary depending on the type of psoriasis. The most common symptoms include red, scaly patches of skin, dry, cracked skin that may bleed, and itching or burning sensations. Some people with psoriasis may also experience joint pain and stiffness – a condition known as psoriatic arthritis.
According to the National Psoriasis Foundation (NPF), it is estimated that around 2% of the Australian population, or approximately 446,000 people, have psoriasis².
Types of psoriasis
There are several types of psoriasis, each with its own set of symptoms and characteristics. The most common types include:
Plaque psoriasis
This is the most common type of psoriasis, characterised by raised, red, scaly patches of skin called plaques. These plaques most commonly appear on the scalp, elbows, knees, and lower back.
Guttate psoriasis
A form of psoriasis characterised by small, red, scaly spots that typically appear on the torso and limbs. Guttate psoriasis is more common in children and young adults and is often triggered by a streptococcal infection.
Inverse psoriasis
This type of psoriasis is characterised by smooth, red, shiny patches of skin that appear in areas of the body that are prone to sweating, such as the armpits, groin, and under the breasts.
Pustular psoriasis
This type of psoriasis is characterised by small, pus-filled blisters on the skin. Pustular psoriasis can be localised to certain areas of the body or can affect large areas of the body.
Erythrodermic psoriasis
A severe and rare form of psoriasis characterised by a widespread, intense redness of the skin and severe scaling. This type of psoriasis can be very serious and requires immediate medical attention.
Psoriatic arthritis
This type of psoriasis affects the joints. It is a form of inflammatory arthritis and can cause pain, stiffness, and inflammation in the joints.
What causes eczema and psoriasis?
Eczema is thought to be caused by a combination of genetic and environmental factors. People with eczema tend to have a genetic tendency to develop the condition, and certain environmental factors such as irritants like soaps and detergents, allergens like pollen or pet dander, and certain fabrics can trigger eczema or make it worse.
Psoriasis is also thought to be caused by a combination of genetic and environmental factors. Many people with psoriasis have a family history of the condition, and it’s believed that certain genetic factors may make some people more susceptible to developing psoriasis. Environmental factors such as stress (need more mindfulness techniques in your life?), infection, injury, smoking, and certain medications can trigger or worsen psoriasis. Research suggests that psoriasis is related to an immune system problem, where the immune system sends the wrong signals to the skin cells, causing them to grow too quickly.
Eczema, psoriasis and autoimmune disease
Eczema and psoriasis are both chronic skin conditions associated with an increased risk of developing an autoimmune disease – a condition in which the immune system mistakenly attacks healthy cells in the body, leading to inflammation and damage.
People with eczema and psoriasis have a higher risk of developing autoimmune diseases such as rheumatoid arthritis, lupus, multiple sclerosis, and inflammatory bowel disease. This association is thought to be due in part to the chronic inflammation that occurs in these skin conditions.
Risk factors for eczema and psoriasis?
Both eczema and psoriasis are chronic skin conditions that can affect people of all ages; however, certain people have a higher risk of developing these conditions.
Eczema is more common in children than in adults. People with a family history of eczema, asthma, or allergies are at a higher risk of developing the condition. Other factors that can increase the risk of eczema include having sensitive skin, exposure to certain irritants or allergens, and certain medical conditions such as hay fever or asthma.
Psoriasis typically develops in adults; however, it can occur in children. People with a family history of psoriasis are at a higher risk of developing the condition, as are people with HIV or other autoimmune diseases, such as rheumatoid arthritis. Other factors that can increase the risk of psoriasis include smoking, obesity, stress, certain infections, and certain medications.
Eczema and psoriasis triggers
Common eczema triggers include:
- Irritants such as soaps, detergents, and certain fabrics
- Allergens such as pollen, pet dander, and dust mites
- Dry skin
- Stress
- Hormonal changes
- Temperature changes
- Certain foods and drinks
- Certain medical conditions, such as hay fever or asthma
Common psoriasis triggers include:
- Stress
- Injuries to the skin, such as a cut or scrape
- Certain medications, such as beta-blockers, and antimalarials
- Infections, such as strep throat
- Cold weather
- Heavy alcohol consumption
- Smoking (find out how to quit smoking)
- Obesity
- Certain skin infections
It is important to note that triggers can vary for each individual, and not everyone with eczema or psoriasis may have the same triggers. Identifying and avoiding triggers can help to manage eczema and psoriasis symptoms.
How are eczema and psoriasis diagnosed?
Eczema and psoriasis are typically diagnosed based on the appearance and location of the rash, as well as a person’s medical history. A dermatologist may also perform a skin biopsy to confirm the diagnosis, and blood tests may be performed to rule out other conditions.
How are eczema and psoriasis treated?
Treatment for eczema and psoriasis often involves a combination of topical medications, oral medications, light therapy, and lifestyle changes.
Eczema treatments
Eczema treatment typically consists of a variety of moisturising, avoiding triggers, and using medications. Some common eczema treatments include:
Moisturiser
Keeping the skin moisturised is essential to eczema management. Simply applying a moisturiser immediately after bathing or showering and throughout the day as needed is the trick to keep eczema symptoms under control.
Avoiding triggers
Identifying and avoiding things that trigger eczema can help reduce flare-ups.
Topical medications
Topical medications applied directly to the skin are often used to treat eczema. These include:
- Topical corticosteroids reduce inflammation and itchiness and are available in creams, ointments, and lotions of different strengths.
- Calcineurin inhibitors help to reduce inflammation and relieve symptoms and are available in cream or ointment form.
- Moisturising creams and ointments help to keep the skin moisturised and prevent dryness.
Light therapy
Also known as phototherapy, light therapy is often used to treat moderate to severe eczema. Light therapy can be self-performed at home or by a dermatologist in a clinic.
Oral medications
Medications, such as immunosuppressants, may also be prescribed for severe cases of eczema.

Psoriasis treatments
Normally a combination of medications, lifestyle changes, and avoiding triggers can be used to treat psoriasis.
Topical medications
These are medications that are applied directly to the skin. They include:
- Topical corticosteroid creams reduce inflammation and itchiness and are available in creams, ointments, and lotions of different strengths.
- Vitamin D analogues slow down the growth of skin cells and are available in cream, ointment, and gel form.
- Retinoids slow down the growth of skin cells and reduce inflammation. They are available in cream, ointment, and gel form.
Light therapy
Like eczema, light therapy is often used to treat moderate to severe psoriasis. It can be performed by a dermatologist or self-administered at home with a specially designed light device.
Oral or injectable medications
- Immunosuppressant medications reduce inflammation and slow skin cell growth.
- Retinoid medications slow down the growth of skin cells and reduce inflammation.
- Biologics are medications made from proteins designed to target specific parts of the immune system involved in psoriasis.
Lifestyle changes
Maintaining a healthy diet and exercise routine, managing stress, and avoiding smoking and excessive alcohol consumption can help improve symptoms of psoriasis.
Avoiding triggers
Identifying and avoiding things that trigger psoriasis can help reduce skin symptoms and psoriasis flare-ups.
It’s important to work with a dermatologist to find the best treatment plan as it varies from person to person, and some treatments may not be covered by Australian health insurance.