Acne manifests in various forms, each with its unique characteristics and treatment approaches. In this comprehensive guide, we delve into the different types of acne, from mild comedonal acne, commonly seen as blackheads and whiteheads, to more severe forms like cystic acne, known for its deep, painful cysts.
Understanding these types can be helpful in identifying the most effective treatment strategies and achieving clearer, healthier skin. Whether you’re a teenager grappling with hormonal changes or an adult facing persistent acne issues, this guide offers valuable insights into the diverse acne types and their treatment – from acne face wash to acne skin care and prescription acne medications.
Overview of Acne: Understanding the Basics
Acne, a widespread skin condition, affects individuals of all ages, though it’s particularly prevalent among teenagers and young adults. It develops when hair follicles become clogged with dead skin cells and excess oil, leading to various types of acne. The severity of acne can range from mild forms, like noninflammatory blackheads and whiteheads, to more severe forms, including inflammatory acne, cystic acne, and nodular acne. Understanding acne is essential for effective acne treatment, as it can manifest differently on each individual’s skin.
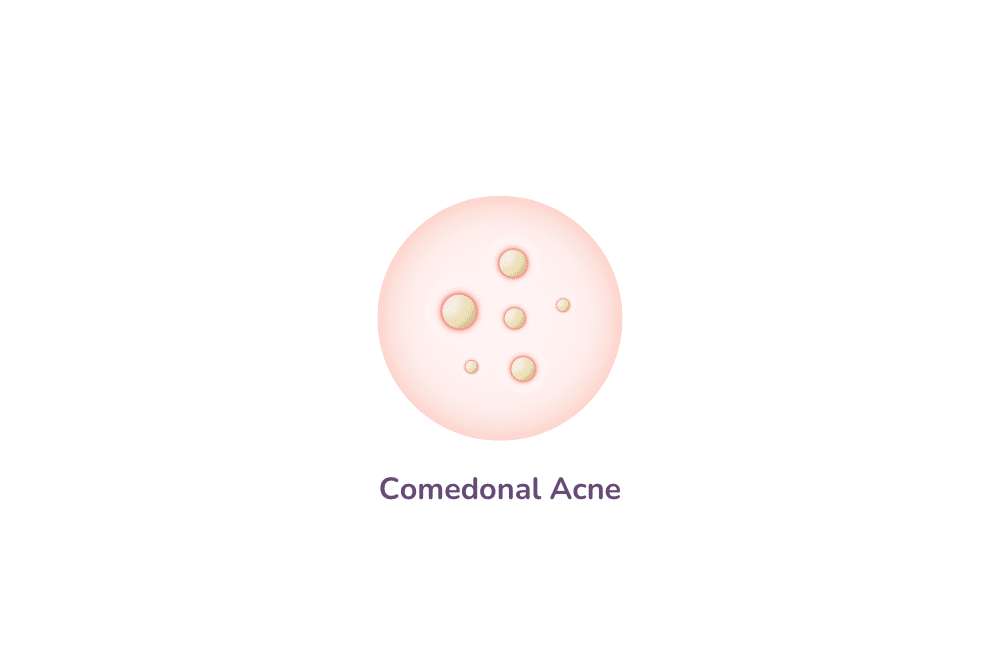
Comedonal Acne: Identifying Blackheads and Whiteheads
Comedonal acne is a form of mild to moderate acne characterised by noninflammatory lesions, primarily blackheads and whiteheads. These acne blemishes occur when hair follicles get blocked with a mixture of dead skin cells and excess oil. Blackheads, known for their open, dark surface, form when the clogged pore is exposed to air. In contrast, whiteheads are closed comedones, where the clogged hair follicle remains beneath the skin, resulting in a small, flesh-coloured bump.
This type of mild acne is particularly common among teenagers and young adults, often triggered by hormonal changes and an increase in sebum production. While considered a milder form of acne, comedonal acne can still be bothersome and may require acne treatment.
Over-the-counter medications containing salicylic acid or benzoyl peroxide are often effective in treating this type of acne lesion, as they help break down the blockage within the pores and reduce excess oil. For persistent cases, prescription acne medications might be recommended. Maintaining a regular skincare routine that includes gentle cleansing can also prevent the buildup of dead skin cells and excess oil, reducing the likelihood of developing comedonal acne.
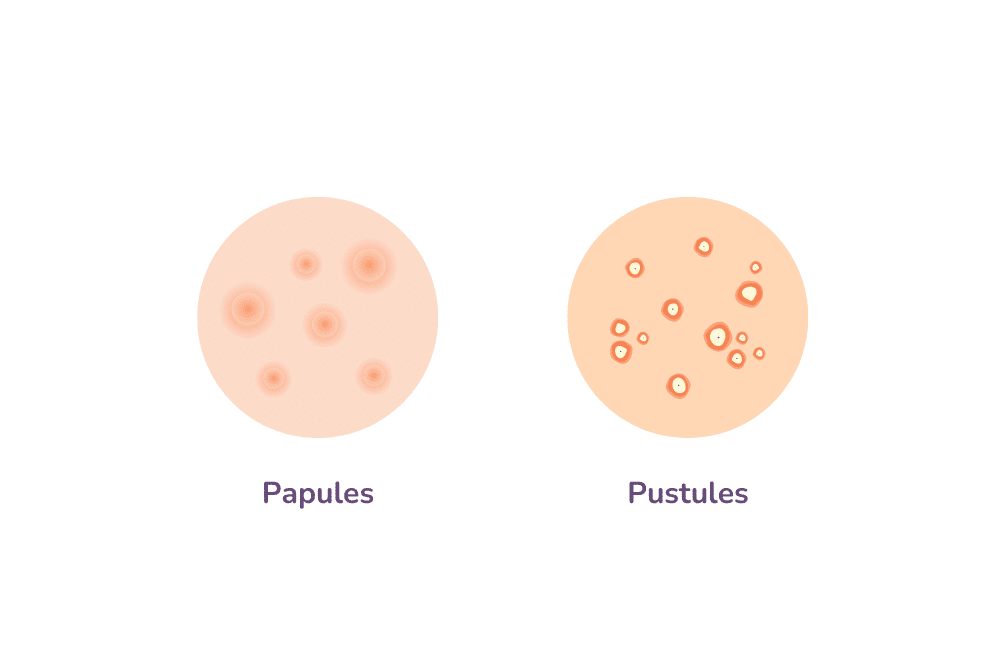
Inflammatory Acne: From Papules to Pustules
Inflammatory acne is a more severe form of acne characterised by red, swollen, and often painful lesions. This condition arises when the clogged pores become infected with bacteria, leading to inflammation. The most common types of inflammatory acne are papules and pustules. Papules are small, pink bumps that can feel tender to the touch, indicating an infection beneath the skin’s surface. Pustules, on the other hand, are similar in size but filled with pus (basically pus-filled pimples), giving them a white or yellow appearance.
Treating inflammatory acne often involves a combination of over-the-counter and prescription medications. Benzoyl peroxide is a popular over-the-counter option for its antibacterial properties, which help reduce the presence of acne-causing bacteria. Salicylic acid is another effective ingredient, aiding in the exfoliation of dead skin cells to prevent clogged pores. For more severe cases, dermatologists may prescribe antibiotics to reduce inflammation and fight bacterial infection. In some instances, hormonal acne treatment options like birth control pills or other hormonal therapies may be considered, especially if the acne is linked to hormonal changes such as those experienced during the menstrual cycle.
It’s important to approach inflammatory acne treatment with care, as aggressive or inappropriate treatment can lead to acne scars. Gentle skincare routines and avoiding the temptation to pick or squeeze the lesions can prevent further irritation and reduce the risk of scarring. With the right combination of treatments, most people see a significant improvement in their inflammatory acne.
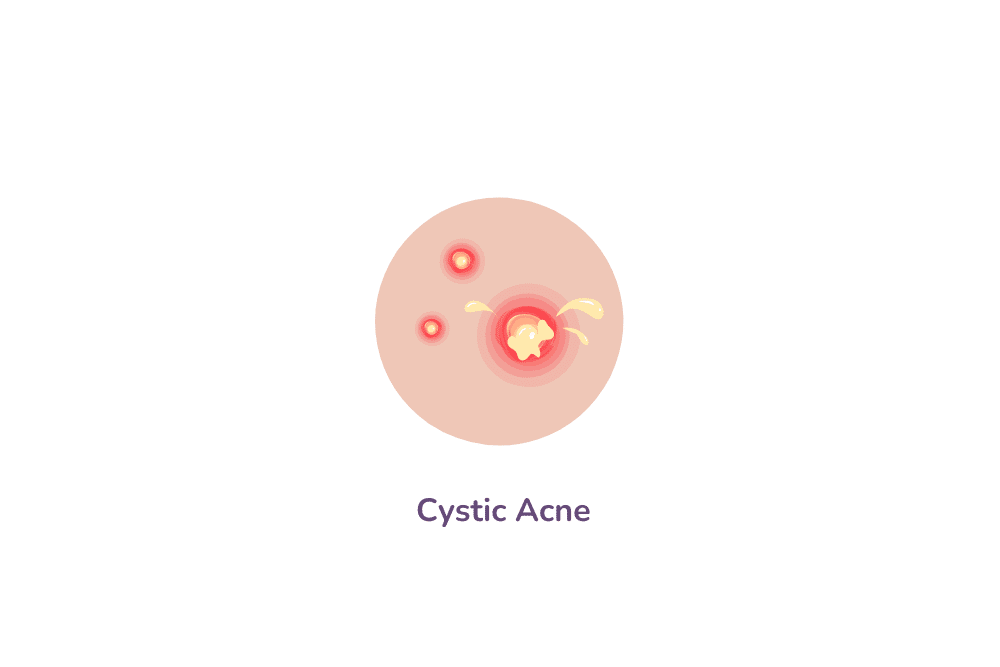
Cystic and Nodular Acne: Managing Severe Skin Conditions
Cystic acne and nodular acne represent the most severe forms of acne, characterised by deep, inflamed, and often painful lesions. Cystic acne involves large, pus-filled cysts that form deep within the skin, leading to significant discomfort and a higher risk of scarring. Nodular acne, similarly, features hard, painful lumps under the skin’s surface. Both nodules and cysts result from clogged hair follicles by dead skin cells, excess sebum, and bacteria.
Managing these severe skin conditions often requires a more aggressive treatment approach. Over-the-counter medications typically are not effective for cystic and nodular acne due to the depth and severity of the lesions. Instead, dermatologists commonly prescribe oral antibiotics to reduce inflammation and combat bacterial infection. In some cases, a powerful prescription medication is used for its ability to dramatically reduce sebum production, although it comes with a significant risk of side effects and is typically used as a last resort.
Hormonal treatments may also be effective, particularly in cases of hormonal acne, which is often linked to fluctuations in hormones during events like the menstrual cycle. Additionally, corticosteroid injections can be used to rapidly reduce swelling and promote healing in specific, severely inflamed cysts or nodules.
Due to the potential for acne scarring and the complex nature of cystic and nodular acne, it’s important for individuals suffering from these conditions to seek professional medical advice. Treatment plans often include a combination of prescription acne medications, lifestyle changes, and, in some cases, professional skin care treatments. Early intervention is key to reducing the risk of long-term scarring and achieving clearer skin.
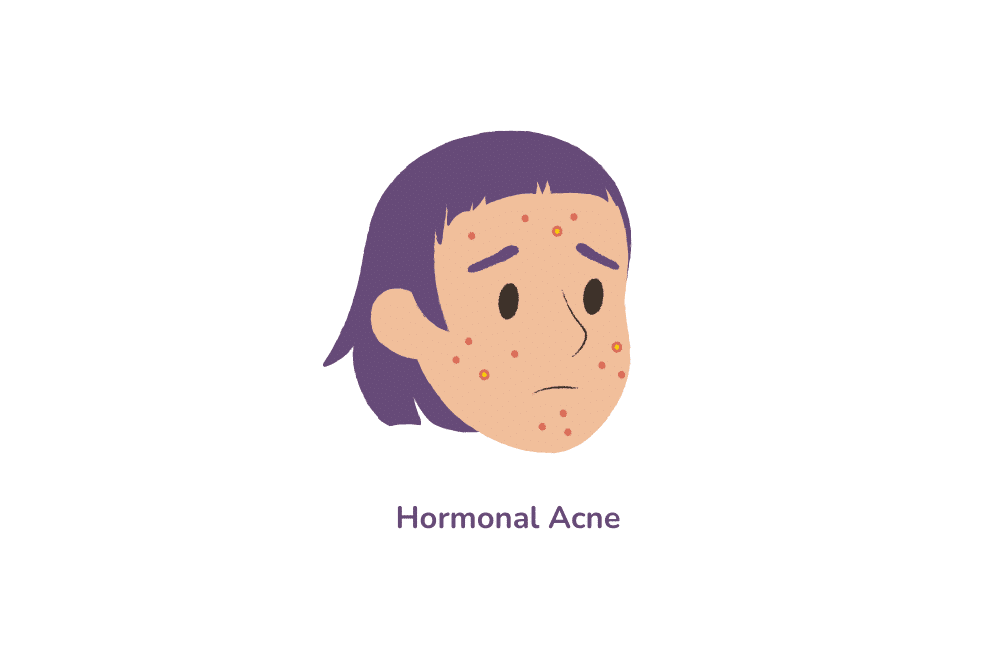
Hormonal Acne: The Impact of Hormones on Skin Health
Hormonal acne is a skin condition primarily influenced by fluctuations in hormones. It commonly occurs during puberty but can persist or appear for the first time in adulthood, especially in women during menstrual cycles, pregnancy, or due to conditions like polycystic ovary syndrome (PCOS). This type of acne blemish is typically characterised by its location on the lower face, jawline, and chin, and can range from mild comedonal acne to severe cystic acne lesions.
The primary culprit in hormonal acne is an excess of androgens, hormones that can increase the size and activity of sebaceous glands, leading to excess oil production. This excess oil, in combination with dead skin cells, can lead to clogged pores, creating an environment where acne-causing bacteria thrive.
Treating hormonal acne often requires a different approach compared to other acne types. Over-the-counter treatments like salicylic acid and benzoyl peroxide may help with surface lesions, but for deeper, hormone-driven acne, other strategies are often necessary. Prescription medications, such as hormonal birth control pills or anti-androgen drugs, can be effective in balancing hormone levels and reducing acne outbreaks.
In addition to medication, lifestyle changes can also play a significant role in managing hormonal acne. This includes maintaining a consistent skincare routine, reducing stress (as stress can exacerbate hormonal fluctuations), and considering dietary changes. Foods with a high glycemic index, for instance, can trigger hormonal changes that may worsen acne.
Since hormonal acne is often linked to internal factors, consulting a dermatologist or healthcare provider is important for an accurate diagnosis and effective treatment plan. They can offer personalised advice and potentially prescribe medication tailored to the individual’s specific hormonal profile and skin condition.
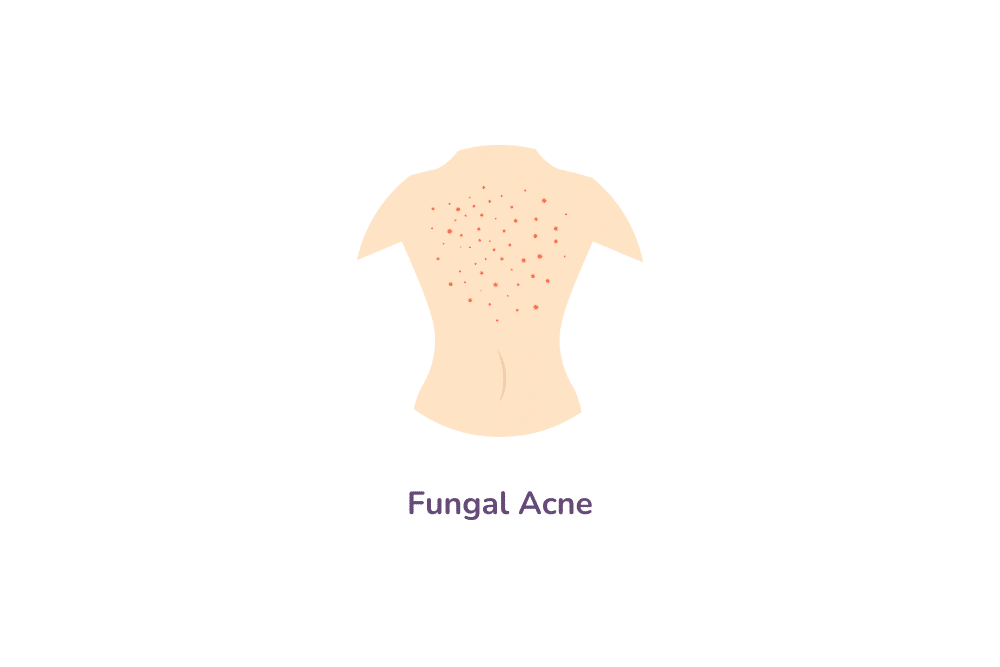
Fungal Acne: Understanding and Managing the Condition
Fungal acne, medically known as Pityrosporum folliculitis or Malassezia folliculitis, is often mistaken for traditional acne vulgaris due to its similar appearance. However, it’s caused by an overgrowth of yeast, a type of fungus, in the hair follicles, leading to itchy, uniform, and small pustules often clustered on the chest, back (get rid of back acne with these tips), and shoulders, though they can appear on the face as well.
Unlike typical acne, which is caused by bacteria and excess sebum, fungal acne is triggered by an imbalance in the skin’s microbiome, often exacerbated by humid environments, tight clothing, or a compromised immune system. This condition can also be a side effect of antibiotic use, which disrupts the normal skin flora.
Treating fungal acne requires a different approach than bacterial acne. Over-the-counter dandruff shampoos containing antifungal agents can be effective when applied to the affected areas. Topical antifungals and oral antifungal medications may also be prescribed for more persistent cases.
It’s important to differentiate fungal acne from other types of acne to ensure proper treatment. If you suspect you have fungal acne, consulting with a dermatologist is essential. They can provide a correct diagnosis and recommend an appropriate treatment regimen, which may include changes in acne skin care products and routines to reduce the risk of recurrence. Additionally, maintaining good hygiene, avoiding excessive sweating, and wearing loose-fitting clothes can help prevent fungal acne flare-ups.
Acne Treatment Options: From Over-the-Counter Solutions to Professional Care
The battle against acne involves a wide range of treatment options tailored to different skin types and severities of acne. These options can be broadly categorised into over-the-counter solutions and professional care.
Over-the-Counter Solutions
Topical Treatments
These include products, such as acne face wash and acne creams, containing salicylic acid, benzoyl peroxide, and alpha hydroxy acids. They help exfoliate the skin, unclogging pores, and reducing inflammation.
Cleansers and Moisturisers
Gentle acne skin care products can help maintain skin hygiene without over-drying or irritating the skin.
Natural Remedies
Some individuals find success with natural ingredients like tea tree oil, though their effectiveness can vary.
Professional Care
Prescription Acne Medications
These include topical retinoids, antibiotics, and hormonal treatments like birth control pills or anti-androgens.
Dermatological Treatments
Procedures like chemical peels, laser therapy, and microdermabrasion can be effective, especially for persistent or severe acne.

Understanding Acne Scars: Types and Treatment Strategies
Acne scars, often a sequel to severe forms of acne like cystic acne, vary in appearance and can be broadly categorised into atrophic (depressed) scars, including boxcar, rolling, and ice pick scars, and hypertrophic or keloid (raised) scars.
The choice of treatment depends on the type and severity of the scarring. Options range from topical treatments for mild scarring, which promote skin regeneration and collagen production, to more intensive procedures like chemical peels, laser therapy, and microneedling for deeper scars.
In cases of severe acne scarring, surgical treatments such as subcision or excision may be considered. Consulting with a dermatologist is the key to an appropriate treatment plan, as they can tailor therapies to individual needs and skin types, ensuring both safety and effectiveness in scar management.