Fungal acne, often confused with traditional acne, is caused by an overgrowth of yeast within the hair follicles. The key to treating it lies in using anti-fungal and anti-inflammatory skincare products and avoiding ingredients that exacerbate yeast growth.
Struggling with those pesky, stubborn bumps that just won’t go away? You might be dealing with fungal acne, but don’t worry – there are easy solutions to help you achieve clearer skin! This guide offers simple, effective methods tailored for those battling this unique skin concern, ensuring your journey to smooth, blemish-free skin is just a few steps away.
Understanding Fungal Acne
Fungal acne, technically known as Malassezia folliculitis or Pityrosporum folliculitis, is often mistaken for regular acne vulgaris. Unlike typical acne, which occurs when pores are blocked with dead skin cells, and sebum(oil), fungal acne arises from an overgrowth of yeast within the hair follicles. This yeast, part of the skin’s natural microbiome, usually coexists harmlessly with other skin cells. However, when there’s an imbalance, often in oily skin environments, this yeast thrives, leading to fungal acne breakouts
These breakouts, characterised by small, itchy bumps, are not the same as bacterial acne and thus require different treatment strategies. While regular acne responds well to oral antibiotics and topical treatments targeting bacteria, treating fungal acne involves antifungal creams or dandruff shampoos containing antifungal agents. These products help reduce yeast growth and inflammation in the hair follicles.
Preventing fungal acne involves maintaining a balanced skin environment to deter yeast overgrowth. Simple steps like using gentle, non-oily skincare products and avoiding excess moisture can be effective. For those who experience fungal acne, it’s important to diagnose fungal acne correctly, as mistaking it for bacterial acne can make fungal acne worse, leading to ineffective treatments and prolonged discomfort.
It’s essential to understand the differences between fungal acne vs regular acne to treat and prevent fungal acne effectively. Regular acne, for instance, might respond to oral antifungal medication, but fungal acne typically does not. Understanding these nuances is key to developing a successful fungal acne treatment plan and can help prevent future fungal acne breakouts.

Identifying Fungal Acne Symptoms
Symptom Comparison: Fungal Acne vs Regular Acne
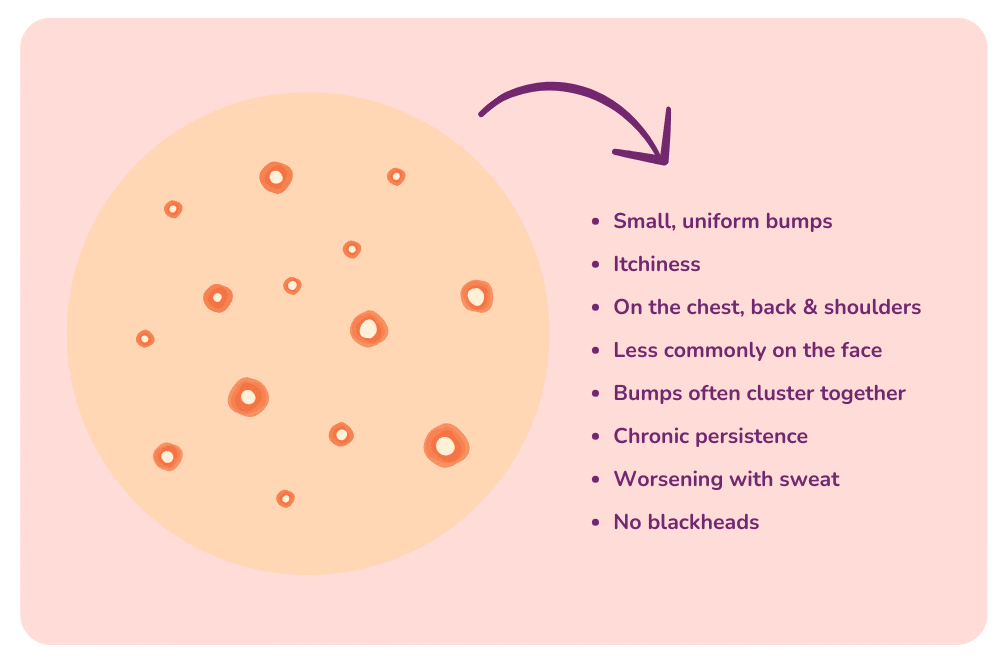
Identifying the symptoms of fungal acne is the key to effective treatment. Unlike typical acne vulgaris, fungal acne appears as uniform, itchy bumps, primarily found in areas dense with hair follicles, such as the forehead, chest, and back (commonly known as back acne). These bumps often worsen with factors like sweat or humidity. A key distinction between fungal and regular acne is the itchiness accompanying the breakouts. Regular acne might cause discomfort or pain, but fungal acne usually presents a persistent itch.
Appearance and Distribution
Fungal acne symptoms include clusters of small, similar-sized bumps, contrasting with the varied size and more sporadic distribution of typical acne. This uniformity in size and clustering is a telltale sign of fungal acne.
Diagnosis and Differentiation
A dermatologist usually diagnoses fungal acne by examining the affected areas and discussing symptoms. Sometimes, a skin scraping may be performed to confirm yeast presence. Correctly differentiating fungal acne from other skin conditions, such as bacterial acne, cystic acne, or yeast infections, is vital for choosing the right treatment.
Recognising Triggers
Understanding and recognising triggers is essential for people prone to developing fungal acne. Triggers can include excessive sweating, humid environments, tight clothing, and using oily skin products that exacerbate yeast growth. Early recognition of these symptoms and triggers can aid in effectively treating and preventing fungal acne.
Effective Treatment Options
Topical Antifungal Treatments
The cornerstone of treating fungal acne involves using topical antifungal treatments. These include over-the-counter antifungal creams, medicated body washes, and shampoos containing active ingredients. These products directly target the yeast within the hair follicles, reducing the fungal overgrowth that causes acne.
Oral Antifungal Medications
In more severe cases, oral antifungal medication may be prescribed when topical treatments are insufficient. Prescription acne medications work systemically to combat yeast overgrowth, offering an effective solution for treating fungal acne, especially in widespread or persistent cases.
Lifestyle and Skincare Adjustments
Lifestyle changes play a big role in managing and preventing fungal acne. This includes wearing loose, breathable clothing, showering after excessive sweating, and avoiding heavy, oily skincare products that can exacerbate yeast growth. Incorporating non-comedogenic, fungal-acne-safe products into your skincare routine can also significantly help.
Alternative Remedies and Preventative Measures
Some people find success with alternative remedies like tea tree oil, known for its natural antifungal properties. However, using these in moderation and alongside proven treatments is important. Preventative measures, such as maintaining a balanced diet and managing stress with mindfulness techniques, can also support the skin’s overall health and reduce the likelihood of fungal acne flare-ups.
Effective treatment of fungal acne is a combination of using the right products, making lifestyle adjustments, and being proactive in skin care. With consistent and appropriate care, managing fungal acne effectively and achieving clearer, healthier skin is possible.
Targeting Fungal Acne on the Face
Treating fungal acne on the face requires specialised skincare products that target yeast overgrowth without irritating sensitive facial skin. Opt for gentle, antifungal facial cleansers and creams formulated with active ingredients. Specific active ingredients help reduce the yeast population on the skin, alleviating fungal acne.
Avoiding Aggravating Factors
It’s important to identify and avoid factors that aggravate facial fungal acne. This includes refraining from using heavy, oil-based makeup and skincare products that can clog pores and promote yeast growth. Switch to non-comedogenic, lightweight products that maintain skin hydration without adding excess oil.
Consistent Skincare Routine
Consistency is key in a skincare routine targeting fungal acne on the face. Regular cleansing, especially after sweating, and applying antifungal treatments as directed can significantly reduce fungal acne outbreaks. Using a separate towel for your face is also important to prevent spreading yeast from other body parts.
Dermatological Treatments and Advice
In cases where over-the-counter treatments are ineffective, consulting with a dermatologist is advisable. They might prescribe stronger antifungal medications or recommend specific treatments like chemical peels or light therapy, which can be beneficial in controlling fungal acne. A dermatologist can also provide tailored advice on managing fungal acne based on skin type and condition.
Addressing fungal acne on the face demands a careful balance of effective treatment, avoiding triggers, and maintaining a consistent, skin-friendly routine. With the right approach, controlling fungal acne and achieving a clearer, healthier complexion is possible.

Banishing Fungal Acne on the Forehead
Tailored Topical Treatments
Fungal acne on the forehead often requires targeted topical treatments. Antifungal creams or gels containing certain active ingredients are effective in curbing yeast overgrowth in this area. It’s essential to apply these treatments consistently as part of your daily skincare routine to see significant improvement.
Hair and Scalp Care
Since the forehead is close to the hairline, proper hair and scalp care is essential in managing fungal acne in this area. Using anti-dandruff shampoo that contains antifungal agents can help reduce yeast spread from the scalp to the forehead. Additionally, avoid using oily hair products that can drip down and worsen fungal acne on the forehead.
Skincare Product Selection
When tackling fungal acne on the forehead, be mindful of your skincare products. Opt for non-comedogenic, oil-free facial products that won’t clog pores or encourage yeast growth. Also, be cautious with makeup and sunscreens, ensuring they suit acne-prone or sensitive skin.
Lifestyle Adjustments
Lifestyle adjustments can also help in banishing fungal acne on the forehead. This includes avoiding tight hats or headbands that can trap sweat and oil, leading to an environment conducive to fungal growth. Regularly washing pillowcases and avoiding touching your forehead with unclean hands can also prevent the spread of yeast and bacteria.
Effectively treating fungal acne on the forehead requires a combination of appropriate topical treatments, careful hair and scalp care, selective use of skin care products, and lifestyle modifications. With these steps, you can successfully manage and reduce fungal acne outbreaks, leading to clearer and healthier skin.

Clearing Up Fungal Acne: Tips and Tricks
Integrating Antifungal Products
Incorporate antifungal products into your skincare regimen. Products like antifungal creams, body wash, or shampoos can be highly effective. Use these regularly, but be mindful not to overdo it, as this can irritate the skin.
Maintaining Hygiene
Good hygiene practices are essential in managing fungal acne. Shower immediately after intense activities that cause sweating, as damp and sweaty skin can exacerbate fungal growth. Use clean towels and change bed linens frequently to reduce the risk of re-infection.
Avoiding Common Triggers
Identify and avoid triggers that can worsen fungal acne, such as tight clothing, humid environments, and oily skincare products. Opt for loose, breathable fabrics and maintain a cool, dry environment as much as possible.
Dietary Considerations
While the link between diet and fungal acne isn’t direct, maintaining a balanced diet can support overall skin health. Some people find that reducing sugar and yeast-containing foods can positively impact their skin condition.
Natural Remedies
Certain natural remedies, such as tea tree oil, have antifungal properties. These can be used in moderation alongside your primary treatment. However, always perform a patch test first to ensure you don’t have a reaction.
Seeking Professional Help
If over-the-counter acne treatments and home remedies aren’t effective, don’t hesitate to have fungal acne diagnosed by a healthcare professional. A dermatologist can provide targeted treatment plans and prescribe stronger antifungal medication if needed.
Consistency is Key
Consistency in your skincare routine is vital for effectively clearing up fungal infections. Stick to your treatment plan, and keep going even if results aren’t immediate. It can take several weeks to see significant improvements.
By following these tips and tricks, you can effectively clear up fungal acne and maintain healthier, clearer skin over the long term.