Many women often have questions about their vulva health, and one common concern is the presence of pimples on the vulva, also known as vaginal pimples. These concerns are natural, and understanding vulva health is key for overall well-being. In this article, we delve into the intricacies of vulva health and specifically address the common concern: “Can you get genital pimples?” By exploring the anatomy, causes, symptoms, and appropriate care, you’ll gain essential information and guidance to ensure your vaginal area remains healthy and free from discomfort. Let’s begin by understanding the basics of vulva health and exploring the common concerns surrounding vulva and vaginal acne.
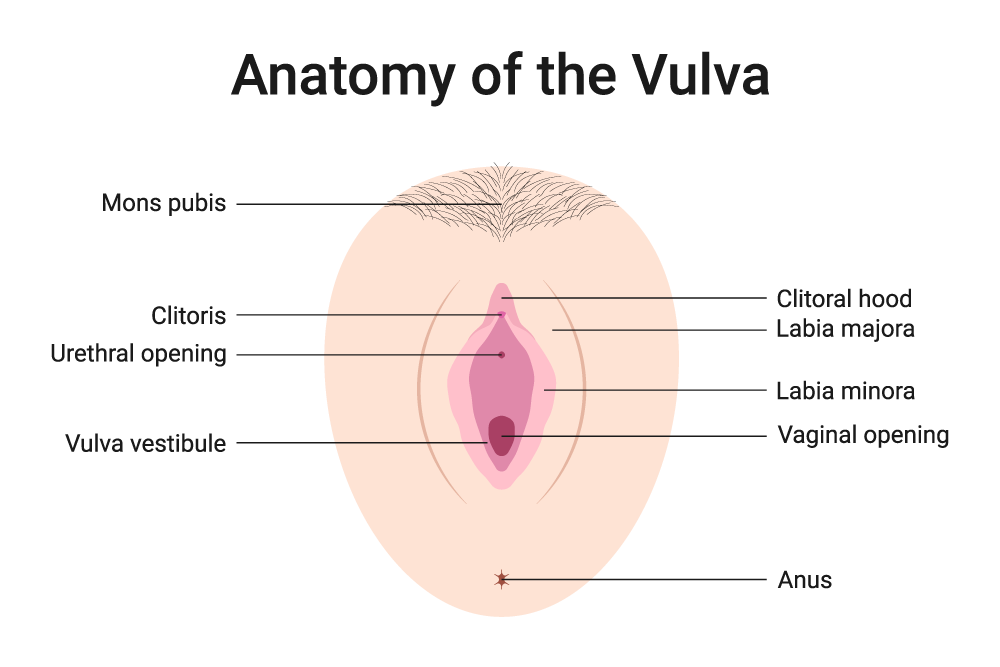
Anatomy of the Vulva
The vulva is an intricate and sensitive region of a woman’s anatomy, featuring a variety of structures that play vital roles in both reproductive and sexual health. By gaining a deeper understanding of the vulva’s structure, one can better appreciate its complexities and potential health concerns.
- Labia Majora: The labia majora, often called the “outer lips,” are the prominent folds of skin that encase the vulva externally. They serve as a protective shield, guarding the delicate inner structures. Typically covered in pubic hair, the labia majora play a crucial role in safeguarding the vulva against external elements and potential injuries.
- Labia Minora: Nestled beneath the labia majora, the labia minora, or “inner lips,” are thinner and more delicate folds of skin. Rich in nerve endings, the labia minora contribute significantly to sexual pleasure and arousal, making them an essential part of sexual health.
- Clitoris: The clitoris is a highly sensitive organ located at the top of the vulva, where the labia minora meet. Its primary function is to facilitate sexual pleasure and arousal, containing thousands of nerve endings that can result in intense sensations when stimulated.
- Vaginal Opening: The vaginal opening is the gateway to the vagina, allowing for various functions such as the passage of menstrual blood, childbirth, and sexual intercourse. It’s a key aspect of reproductive and sexual health; its well-being is vital for overall vulva health.
- Urethral Opening: Found just above the vaginal opening, the urethral opening is where urine exits the body. Maintaining the health of this area is essential to prevent urinary tract infections (UTIs) and ensure proper urinary function.
- Perineum: The perineum is the area between the vaginal opening and the anus. It plays a role in childbirth and sexual pleasure, making it an important part of the vulva’s anatomy.
Understanding the distinct components that make up the vulva is foundational to recognising any changes or issues that may arise, such as vulva pimples.
What Are Vulva Pimples?
Vulva pimples, also known as vulva acne, are small, raised, and often red or flesh-coloured bumps that appear on the vulva. They are similar in appearance to the pimples that occur on other parts of the body, like the face, back, or chest. These pimples can vary in size and may be filled with pus or appear as whiteheads.
How They Differ from Other Bumps
It’s essential to distinguish vulva pimples from other types of bumps or lesions that may appear in the genital area, as their causes and treatments can differ significantly. Here’s how vulva pimples differ from other common genital bumps:
Vulva Pimples vs. Ingrown Hairs
An ingrown hair occurs when a hair follicle becomes trapped beneath the skin’s surface. Ingrown hairs can lead to redness and small bumps that resemble a vaginal pimple. However, ingrown hairs are typically caused by hair removal methods like shaving or waxing. Learn how to shave your vulva to minimise the risk of ingrown hairs.
Vulva Pimples vs. Genital Warts
Genital warts are caused by the human papillomavirus (HPV) and appear as growths or clusters of small, flesh-coloured bumps. They have a different appearance from vulva pimples and may require specific medical treatment.
Vulva Pimples vs. Genital Herpes
Genital herpes is a viral infection spread through sex, and outbreaks can cause painful sores or blisters in the genital area. Genital herpes lesions are distinct from vulva pimples and are often accompanied by flu-like symptoms.
Vulva Pimples vs. Cysts or Boils
Cysts and boils are larger, deeper lumps that can develop beneath the skin’s surface. They are usually painful and may require medical attention.
Causes of Vulva Pimples
Vulva pimples, like pimples elsewhere on the body, can have various underlying causes. Here, we’ll explore some common factors that can lead to the development of pimples on the vaginal area:
Hormonal Changes
Hormonal fluctuations can trigger the appearance of vulva pimples. These changes may occur during:
- Menstrual Cycle: Hormone levels naturally shift during menstruation, sometimes leading to pimples on the vulva.
- Pregnancy: Pregnancy brings significant hormonal changes and some women may experience vulva pimples during this time.
- Puberty: Adolescent girls often go through hormonal changes, which can result in pimples in various areas, including the vulva.
Blocked Pubic Hair Follicles
Like elsewhere on the body, the vulva area has sweat glands and hair follicles that are prone to buildup and blockage. When a hair follicle gets clogged with dead skin cells, oil, or sweat, it can form a pimple. Factors contributing to blocked hair follicles include:
- Shaving or Waxing: Hair removal methods like shaving or waxing can sometimes cause irritation and lead to blocked follicles.
- Tight Clothing: Wearing tight clothing that traps moisture and sweat can contribute to follicle blockages.
Bacterial Infections
Bacterial infections can also be a cause of vulva pimples. These infections may include.
- Folliculitis: This is an infection of the hair follicles and can lead to red, pimple-like bumps on the vulva.
- Staph Infections: Infections caused by Staphylococcus bacteria can occasionally lead to pimple formation.
Allergic Reactions
Allergies to certain products or substances that come into contact with the vulva can lead to irritation and pimples. Potential allergens might include:
- Detergents and Soaps: Some detergents or soaps used for washing underwear or the vulva can cause allergic reactions.
- Latex Allergy: Allergic reactions to latex in condoms or other products can result in vulva irritation.
It’s essential to identify the underlying cause of vulva pimples to determine the most appropriate treatment and preventive measures.
Symptoms and Signs
Recognising vulva pimples is essential for proper care and treatment. Vulva pimples typically exhibit several distinct characteristics:
- Appearance: Vulva pimples appear as small, raised bumps on the vulva. They can range in colour from red to flesh-toned, and some may have a white or yellowish centre, resembling a pimple or whitehead.
- Size: Vulva pimples vary in size but are generally smaller than a pencil eraser.
- Texture: They often have a slightly firm or tender feel when touched, similar to the types of pimples on the face.
- Pain or Discomfort: Vulva pimples can be sensitive or painful, especially if inflamed or infected.
- Itching or Irritation: Some vulva pimples may cause itching or irritation in the surrounding area.
- Pus or Fluid: Pimples with a white or yellowish head may release pus or fluid when squeezed.
Self-Care and Prevention
Taking proactive steps for self-care and prevention is crucial for maintaining vulva health and reducing the risk of vulva pimples. Here are some practical measures to consider:
Good Personal Hygiene Practices
Maintaining good hygiene is fundamental for vulva health. Here’s how to keep your vulva clean:
- Gentle Cleansing: Use a mild, fragrance-free soap or just warm water to clean the genital area. Avoid using harsh or scented products, as they can irritate the skin.
- Front-to-Back Wiping: When using the toilet, always wipe from front to back to prevent the spread of bacteria from the anus to the vulva.
- Regular Showers: Taking frequent showers and wearing clean underwear daily can help keep the vulva clean and free from irritation.
- Avoid Douching: Do not use douches or feminine hygiene sprays, as they can disrupt the natural balance of the vulva and lead to irritation.
Preventing Vulva Pimples
Preventing vulva pimples involves minimising potential triggers and promoting overall vulva health:
- Wear Breathable Fabrics: Choose cotton underwear and loose-fitting clothing to allow for proper ventilation and reduce sweat accumulation.
- Practise Safe Sex: If sexually active, use barrier methods like condoms to prevent sexually transmitted infections (STIs) that can lead to vulva pimples.
- Manage Moisture: Keep the vulva dry and free from excess moisture. Pat the area dry after showering.
- Avoid Irritants: Be cautious with products that come into contact with the vulva, such as detergents, scented pads, or synthetic underwear. Opt for hypoallergenic and fragrance-free options.
Safe Hair Removal Techniques
Hair removal in the vulva area can sometimes lead to irritation and ingrown hairs. If you choose to remove hair, consider these safe techniques:
- Trimming: Trimming the hair with scissors or an electric trimmer is less likely to cause irritation than shaving or waxing.
- Shaving Tips: If you prefer shaving, use a clean, sharp razor, and always shave in the direction of hair growth. Apply a gentle shaving gel or cream to reduce friction.
- Waxing Precautions: If you opt for waxing, ensure a professional does it in a clean and hygienic setting. Avoid waxing if you have sensitive skin or a history of skin reactions.
Incorporating these self-care practices and preventive measures into your routine can promote vulva health and reduce the risk of vulva pimples. However, if you develop vulva pimples or experience persistent discomfort, consult a healthcare provider for appropriate guidance and treatment.

When to Consult a Healthcare Provider
In some cases, vulva pimples may require medical attention. Here are situations in which it’s advisable to consult a healthcare provider:
- Severe Pain or Swelling: If a vulva pimple becomes extremely painful or is accompanied by significant swelling, it may indicate an infection that requires medical treatment.
- Multiple or Recurrent Pimples: If you have multiple vulva pimples or they frequently recur, it’s essential to rule out underlying medical conditions or infections.
- No Improvement: If home remedies and OTC treatments do not improve after a reasonable period, consult a healthcare provider for a thorough evaluation.
- Other Symptoms: If you experience additional symptoms such as fever, chills, or flu-like symptoms along with vulva pimples, it may signal a more significant issue.
- Uncertain Diagnosis: If you’re unsure whether a bump is a vulva pimple or if you suspect it might be a different type of lesion, consult a healthcare provider for a proper diagnosis.
Remember that healthcare providers are experienced in addressing these concerns and can offer guidance, perform necessary examinations, and recommend appropriate treatments. Your health and comfort are the top priorities when dealing with vulva pimples or any related issues.
The Importance of Vulva Health Awareness
Awareness of vulva health is not merely a matter of aesthetics; it is a fundamental component of reproductive and sexual health. The vulva is a complex and sensitive part of the female anatomy, and being attuned to its well-being can help detect and manage potential issues early. By demystifying concerns like vulva pimples, we reduce anxiety and encourage open discussions about genital health, fostering a healthier, more informed society.