Chlamydia is a common sexually transmitted infection (STI) primarily associated with sexual contact. However, there is a growing curiosity about whether it’s possible to contract chlamydia without engaging in sexual activities.
In this article, we delve into the various transmission routes of chlamydia, exploring scenarios beyond sexual intercourse that may put individuals at risk. In women, untreated chlamydia can cause pelvic inflammatory disease (PID), ectopic pregnancy and infertility, so understanding the potential non-sexual transmission pathways is crucial for promoting awareness and adopting preventive measures to safeguard your sexual health.
Chlamydia Transmission: Beyond Sexual Intercourse
Chlamydia is commonly associated with sexual activity.
However, the scope of its transmission extends beyond conventional sexual intercourse, prompting a closer look at alternative routes. By understanding the non-sexual modes of transmission, you can better protect yourself and contribute to public health initiatives. Here’s a detailed exploration of how chlamydia can be transmitted beyond the boundaries of vaginal or anal sex:
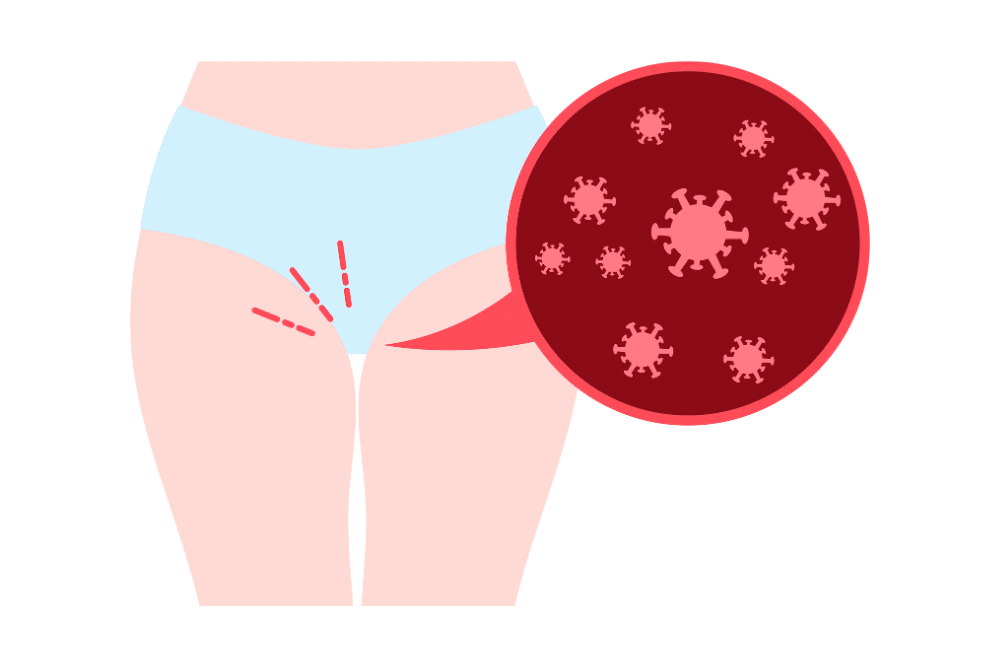
Shared Items and Surfaces
Chlamydia can survive on surfaces for varying durations, creating the potential for transmission through shared items such as towels, sex toys, or even toilet seats. While the risk is considered low, it’s important to maintain good personal hygiene and cautious use of shared objects.
Maternal Transmission during Childbirth
Newborns can contract chlamydia during delivery if the mother is infected. This emphasises the significance of prenatal screenings and treatment to prevent perinatal transmission, highlighting the interconnectedness of sexual health with reproductive health.
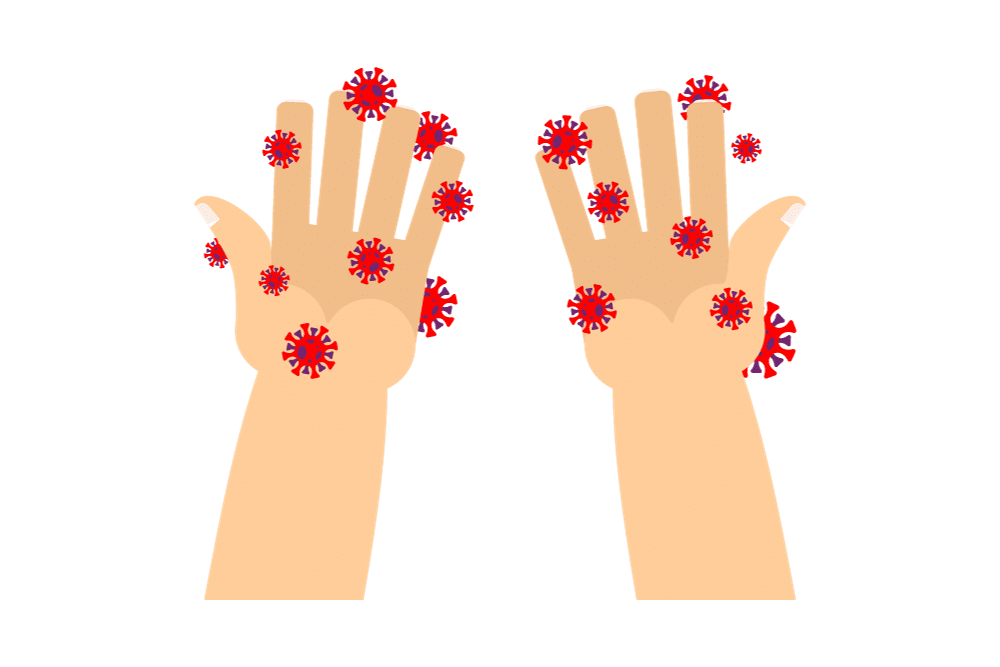
Hand-to-Eye Transmission
Though less common, chlamydia can be transmitted through contact with infected genital secretions and subsequent contact with the eyes. Consider this your reminder of the importance of hand hygiene, particularly after any contact with potentially contaminated areas.
Respiratory Transmission
Chlamydia can also spread through respiratory secretions, primarily in crowded or close-contact environments. This non-sexual transmission mode is another factor to consider in understanding the broader dynamics of how the infection can be contracted.
Autoinoculation
Autoinoculation, or self-infection, is a rare but documented phenomenon where an individual can transfer the infection from one part of the body (e.g., genitals) to another (e.g., eyes or throat) through contaminated hands. Again, this stresses the significance of maintaining good personal hygiene practices.
Chlamydia and Oral Sex: What You Need to Know
While oral sex is often perceived as a lower-risk activity for sexually active individuals, symptoms of chlamydia can still be transmitted through this intimate practice. Understanding the dynamics of chlamydia transmission via oral sex is vital for those seeking to protect their sexual health and stay free of common sexually transmitted infections. Here’s what you need to know about oral sex and STIs:
Oropharyngeal Chlamydia Infections
Chlamydia can infect the oropharynx (throat), leading to oropharyngeal chlamydia. Engaging in oral sex with an infected person can result in the transmission of the bacteria to the throat, causing symptoms of chlamydia such as a sore throat or discomfort.
Asymptomatic Nature
One challenge with oropharyngeal chlamydia is its often asymptomatic nature. Individuals may carry the infection without showing noticeable signs, making regular STI screenings crucial for early detection to avoid untreated chlamydia.
Risk Factors
Certain factors increase the risk of chlamydia transmission during oral sex, such as having multiple sexual partners, engaging in unprotected oral sex, or having a history of other STIs. Being aware of these risk factors can help you make informed decisions about your sexual health.
Prevention and Protection
Using barrier methods such as dental dams or condoms during oral sex can significantly reduce the risk of chlamydia transmission. Open communication with sexual partners about STI testing and maintaining regular screenings are essential components of responsible sexual health practices.
Testing and Treatment
If there’s a concern about potential exposure to chlamydia through oral sex, seeking prompt testing is crucial. Testing methods may include throat swabs; if diagnosed, antibiotics are typically prescribed for effective treatment.
Comprehensive Sexual Health Education
Promoting comprehensive sexual health education is paramount. Many individuals may not be aware of the potential for chlamydia transmission through oral sex, emphasising the need for accessible information and resources.
Unveiling Non-Sexual Chlamydia Transmission
Chlamydia often prompts discussions around sexual activities. However, it’s essential to recognise that chlamydia can be transmitted through non-sexual means. By unveiling these non-sexual transmission pathways, we can better address prevention and foster a more comprehensive approach to public health.
Chlamydia: Not Just a Sexually Transmitted Infection
While often labelled as a sexually transmitted infection, chlamydia’s impact extends beyond the realms of sexual activity.
From mother-to-child transmission during childbirth to fomite transmission on shared objects, understanding the diverse ways chlamydia can be contracted is vital. By recognising that chlamydia is not confined solely to sexual encounters, we can better address preventive measures, promote awareness, and safeguard public health more comprehensively.
Chlamydia Myths Debunked: Non-Sexual Transmission
Chlamydia, often shrouded in myths and misconceptions, is commonly associated with sexual transmission. However, it’s crucial to dispel the notion that this infection is solely a result of intimate encounters. So, we debunk chlamydia myths related to non-sexual transmission, aiming to provide clarity on how this infection can spread beyond conventional expectations.
Myth 1: Chlamydia Is Exclusively Sexually Transmitted
Contrary to popular belief, chlamydia is not limited to sexual transmission alone. While sexual contact is a primary mode of transmission, understanding alternative pathways is crucial. Non-sexual routes, including perinatal transmission, contact with contaminated surfaces, and respiratory transmission, dispel the myth that chlamydia is exclusively linked to sexual activities.
Myth 2: Newborns Can Only Contract Chlamydia Sexually
One prevalent misconception surrounds the transmission of chlamydia to newborns. While sexual transmission is a concern, perinatal transmission during childbirth is a well-documented non-sexual route.
Myth 3: Chlamydia Cannot Survive Outside the Body
Chlamydia can, in fact, survive outside the human body on surfaces for varying periods. This challenges the misconception that bacteria are highly fragile and underscores the importance of personal hygiene and avoiding shared items to prevent potential transmission.
Myth 4: Hand-to-Eye Transmission Is Insignificant
The myth that hand-to-eye transmission of chlamydia is negligible is debunked by the fact that infected genital secretions can lead to ocular infections. Acknowledging this risk highlights the importance of hand hygiene in minimising the chances of unintentional transmission.
Myth 5: Chlamydia Can Only Infect Genital Areas
Chlamydia’s ability to infect various body parts challenges the myth that it exclusively targets genital areas. Autoinoculation, where the infection can be transferred from one part of the body to another, reinforces the need for comprehensive personal hygiene to prevent self-infection.
Exploring Chlamydia Transmission Routes Beyond Sex
Beyond its well-established association with sexual transmission, chlamydia reveals a more intricate web of potential routes for infection.
Maternal transmission during childbirth emerges as a significant non-sexual route, emphasising the importance of addressing maternal health in preventing perinatal infections. Additionally, shared items and surfaces play a role, challenging the notion that chlamydia is exclusively contracted through direct sexual contact.
The exploration also navigates through hand-to-eye transmission, respiratory routes, and the intriguing concept of autoinoculation, shedding light on how this infection can be transmitted outside traditional sexual contexts. Understanding these non-sexual transmission routes is essential for public health initiatives, as it allows for a more comprehensive approach to prevention, education, and the overall management of chlamydia infections in diverse populations.
Non-Sexual Chlamydia Transmission: Fact or Fiction?
Research has unveiled scenarios where chlamydia can be transmitted through shared items, maternal-child transmission during childbirth, and even hand-to-eye contact.
As we navigate this nuanced landscape, it becomes evident that considering chlamydia as solely a sexually transmitted infection may overlook crucial aspects of its potential spread. The blurred lines between fact and fiction in non-sexual transmission underscore the need for continued research, comprehensive sexual education, and open dialogue to dispel myths and promote accurate information surrounding chlamydia.