If you’ve found yourself dealing with recurrent urinary tract infections (UTIs), you’re not alone. Frequent UTIs, also known as chronic UTIs, can be frustrating and uncomfortable. Understanding why they keep happening is the first step towards finding UTI relief.
In this article, we delve into the complexities of recurrent UTIs and explore the risk factors that contribute to recurring UTIs. Whether you’re looking for strategies to prevent urinary tract infections or seeking answers to this groundhog health condition, we’ve got you covered.
But first, what is a UTI?
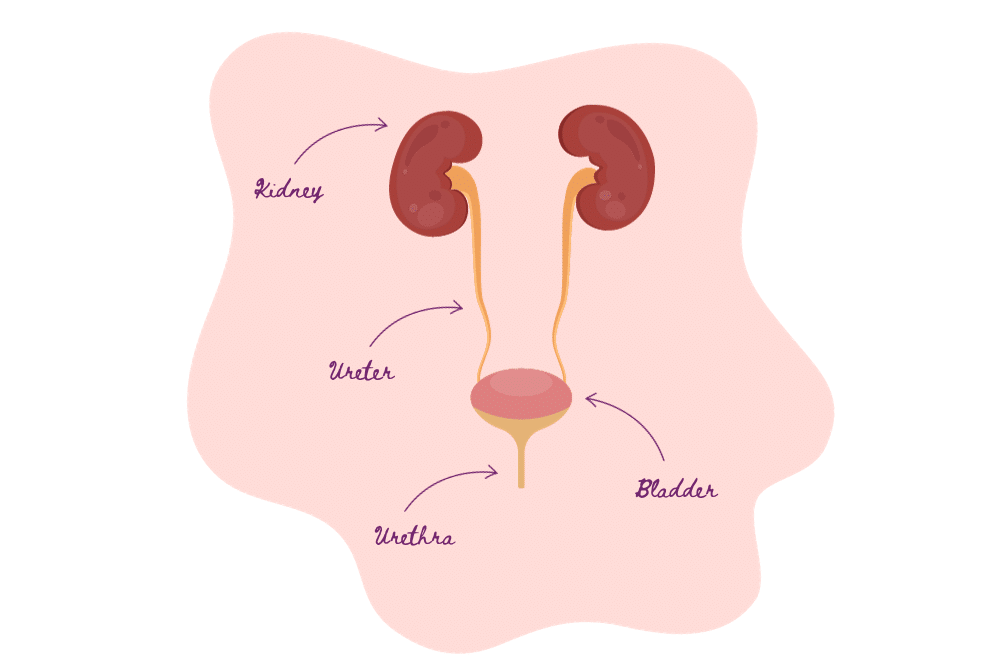
A urinary tract infection is a common medical condition characterised by the presence of bacteria in the urinary system. This infection can affect various parts of the lower urinary tract, including the bladder, urethra, and kidneys, in more severe cases. UTIs typically occur when bacteria from the gastrointestinal tract, such as Escherichia coli (E. coli), enter the urinary system through the urethra. Once inside, these bacteria can multiply and lead to various symptoms, including a frequent and urgent need to urinate, a burning sensation during urination, cloudy or bloody urine, and discomfort or pain in the lower abdomen.
What’s the deal with recurring UTIs?
Recurring UTIs, or recurrent urinary tract infections, can be frustrating and often raise concerns among those who experience them. The main issue with recurring UTIs is that they involve multiple episodes of infection within a relatively short period, which can lead to discomfort, inconvenience, and potential complications if left untreated. Now, let’s explore risk factors that contribute to recurrent UTIs.
The Role of Gender: Why Are Women More Prone to UTIs?
Urinary Tract Infections can be a real pain – literally and figuratively. For many women, UTIs are an all-too-familiar occurrence. But have you ever wondered why they affect women more often than men? Here’s the lowdown on why women tend to be more susceptible to recurring infections:
- Anatomy: It comes down to the urethra. Think of the urethra as a tiny tube that carries urine from the bladder to the outside world. In women, this tube is shorter, making it easier for bacteria to travel from the outside into the bladder, causing infections.
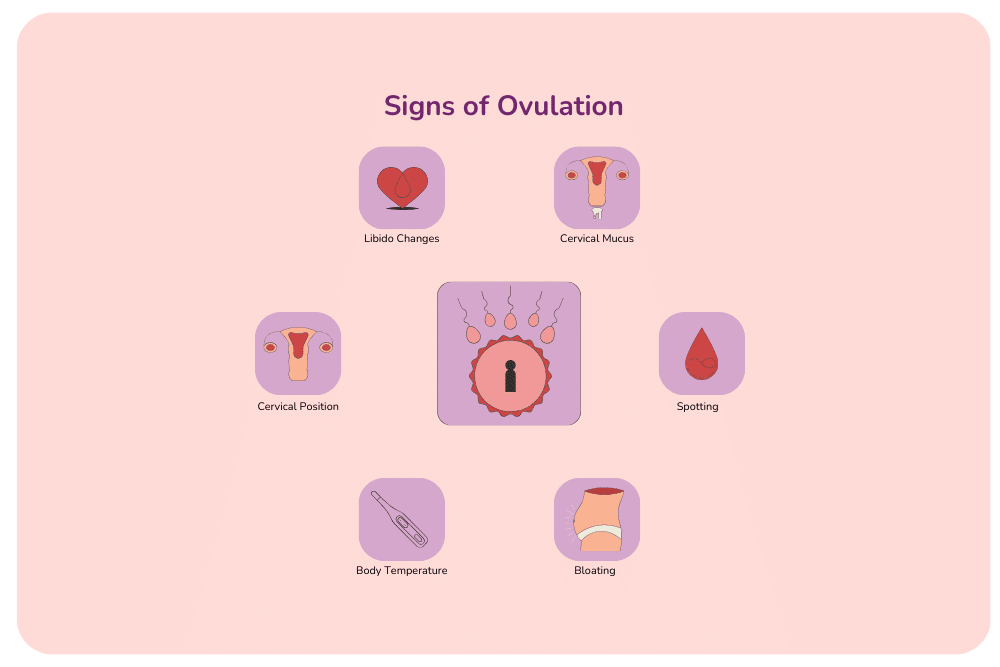
- Hormones at Play: Women experience hormonal fluctuations throughout their menstrual cycle. These changes can impact the balance of bacteria in the urinary tract, potentially making it more hospitable to UTI-causing bacteria. It’s like a temporary vulnerability that occurs at different times during the month.
- Pregnancy and Menopause: Pregnancy and menopause are two big events in a woman’s life. They both bring about significant hormonal shifts. These changes can weaken the muscles around the bladder and affect the pH balance in the urinary tract, creating conditions that are more conducive to UTIs.
Anatomy Matters: Short Urethra and UTIs
One of the primary reasons women are more likely to develop UTIs is their anatomy, specifically the length of the urethra. Let’s dive deeper into this topic to understand how the size of this tiny tube plays a pivotal role in UTI susceptibility.
The Woman’s Urethra: A Vital Connection
The urethra is the exit route for urine and the gateway through which bacteria can enter the urinary tract. This tube is only a few centimetres long in women but significantly longer in men. This shorter path means bacteria have a shorter journey to the bladder, increasing the chances of infection.
Why a Short Urethra?
Evolutionary biology has shaped the female anatomy to accommodate the needs of reproduction. Having a shorter urethra helps protect the reproductive organs, but it inadvertently makes it easier for bacteria to enter the urinary tract.
The Bacteria’s Path
Bacteria from the perineal and anal areas, where they naturally reside, can migrate up the urethra. In women, the shorter urethra means bacteria don’t have to navigate a lengthy path, making it easier for them to reach the bladder and potentially cause an infection. Picture a one-lane road. The road to the bladder is long and winding in men, making it tougher for bacteria to travel. It’s a short, straight strip in women, meaning bacteria can reach the bladder more quickly.
Sexual Activity and UTI Recurrence
Frequent sexual intercourse is one of the common triggers for UTIs, and understanding its role in recurrent infections is essential. When engaging in sexual intercourse, bacteria from the genital area can enter the urethra, increasing the risk of UTIs. While this risk exists for all genders, it’s particularly relevant for women due to their shorter urethra and proximity of the urethral opening to the anus.
Proper hygiene before and after intercourse, including peeing after sex, can help flush out potential troublemakers and reduce the likelihood of infection. Moreover, discussing UTI prevention strategies with your partner, such as using lubricants without irritants and maintaining good personal hygiene, can contribute to a healthier, UTI-free intimate life.
Birth Control Methods and Their Impact on UTIs
Choosing a birth control method is a major decision for women, not only for family planning but also for considering its potential impact on urinary tract infections. Here, we explore how different birth control methods can influence the risk of UTIs:
- Oral Contraceptives (The Pill): The contraceptive pill contains hormones to prevent pregnancy. While it doesn’t directly cause UTIs, the pill can cause fluctuations in hormone levels, which may indirectly influence UTIs by altering the balance of good and bad bacteria in the urinary tract. Some women might experience an increased risk due to these hormonal changes.
- Condoms: Condoms are barrier methods that prevent sperm from reaching the egg and offer protection against sexually transmitted infections (STIs). They have no direct impact on UTIs.
- Intrauterine Device (IUD): IUDs are hormone-based or copper-based contraceptive devices that mainly affect the uterus and do not influence the urinary tract’s susceptibility to UTIs.
- Implant: The implant is a hormonal rod inserted under the skin of the arm. It primarily impacts pregnancy prevention and doesn’t directly cause UTIs.
- Depo-Provera (The Shot): The Depo shot is an injection of hormones every three months. Like oral contraceptives, it can indirectly influence UTI risk due to hormonal changes.
- Natural Family Planning: This birth control method involves tracking your menstrual cycle and avoiding intercourse during fertile days. It does not directly affect UTI risk.
- Sterilisation: Sterilisation is a permanent method for women who are sure they do not want to fall pregnant. It does not have a direct impact on UTIs.
It’s important to remember that the impact of birth control methods on UTI risk is often indirect and varies among women. Some women may notice changes in UTI frequency or susceptibility when using hormonal methods, while others may not experience any difference. If you have concerns about UTIs and your chosen birth control method, discussing your options and potential risks with a healthcare provider is wise. They can provide personalised guidance based on your specific circumstances and health history.
Menopause and UTI Risk: A Consideration for the Future
While you may not be close to experiencing menopause now, keeping this phase of life in mind as you age is essential. Menopause, typically occurring in your late 40s or early 50s, is a natural biological process that marks the end of your reproductive years. One significant aspect of menopause is the dramatic drop in oestrogen levels, which can have various effects on the body, including an increased risk of urinary tract infections (UTIs).
Oestrogen plays a vital role in maintaining the health of your urinary tract. It helps keep the lining of the urethra and bladder strong and well-hydrated, making it more challenging for bacteria to take hold and cause infections. As oestrogen levels decline during menopause, the urinary tract becomes more vulnerable to UTIs.
Understanding this potential risk is key for long-term health planning. While you may not be facing menopause right now, being aware of the changes for menopausal and postmenopausal women can help you to proactively consider preventative measures. As you age, discussing strategies with your healthcare provider, such as hormone replacement therapy or lifestyle adjustments, can help mitigate the increased risk of UTIs associated with menopause.
Wiping Habits and Preventive Measures
Good hygiene practices are essential in reducing the risk of urinary tract infections for women. These include:
- Wiping from Front to Back: Always remember to wipe from front to back after using the toilet. This simple habit helps prevent bacteria from the anal area from coming into contact with the urethra, reducing the risk of UTIs.
- Gentle Cleansing: Be gentle when cleaning your genital area. Harsh soaps and excessive scrubbing can disrupt the delicate balance of good bacteria in the genital area and irritate the urethra. Opt for mild, unscented cleansers and gentle pat-drying instead of vigorous rubbing. Learn more about how to clean your vagina.
- Stay Hydrated: Drinking enough water is important for overall health and keeping the urinary tract flushed. Adequate hydration helps prevent the buildup of bacteria in the bladder.
- Urinate Before and After Sex: Before and after sexual activity, make it a habit to urinate. This helps flush out any potential bacteria that may have entered the urethra during intercourse.
- Consider Showering After Sex: A brief shower can help wash away any bacteria that may have come into contact with your genital area during intimacy, further reducing the risk of UTIs.
- Wear Cotton Underwear: Cotton underwear is breathable and helps keep the genital area dry, reducing the risk of bacterial growth. Avoid tight-fitting or non-breathable fabrics, as they may create a moist environment conducive to UTIs.
Incorporating these simple yet effective hygiene practices into your daily routine can help in preventing UTIs. Good wiping habits, gentle cleansing, proper hydration, and proactive measures before and after sexual activity are essential steps in maintaining optimal urinary health. Remember, prevention is key in the fight against UTIs, and these habits can make a world of difference in your well-being.
Hydration: How It Affects UTI Frequency
Hydration is a fundamental aspect of maintaining overall health, and it plays a key role in reducing the frequency of urinary tract infections in women in the following ways:
- Dilution and Flushing: Drinking plenty of water helps dilute urine concentration. This makes it more challenging for bacteria to thrive in the urinary tract. Additionally, adequate hydration supports the flushing of harmful bacteria out of the urinary system.
- Immune System Support: Dehydration weakens the immune system, making it less effective at fighting off infections. Staying hydrated supports your body’s ability to mount a robust defence against UTI-causing bacteria.
- Preventing Urinary Stasis: Hydration helps prevent urinary stasis, where urine stagnates in the bladder. When urine lingers in the bladder, it becomes a breeding ground for bacteria.
Hydration Tips
To stay well-hydrated, aim to drink at least eight glasses of water a day and more if you’re physically active or in a hot climate. Pay attention to your body’s thirst signals, and choose water as your primary beverage.
Both caffeine and alcohol have diuretic effects, which means they can increase urine production and potentially lead to dehydration if not offset by drinking water. Be mindful of your consumption and try to hydrate when consuming these beverages.
Staying well-hydrated is a simple yet highly effective way to reduce the frequency of UTIs. By diluting urine, supporting your immune system, preventing urinary stasis, and following hydration tips, you can create an environment that is less favourable for UTI-causing bacteria in your urinary tract. Incorporating these practices into your daily routine is a proactive step toward maintaining optimal urinary health.
The Connection Between UTIs and Antibiotic Use
Urinary Tract Infections are common, and antibiotic use is a standard treatment. However, a complex relationship between UTIs and antibiotics is important to understand.
- UTI Treatment Heroes: Antibiotics are medications used to treat bacterial infections, including UTIs. They work by killing or inhibiting the growth of the bacteria causing the infection.
- Overuse and Antibiotic Resistance: Overusing antibiotics by taking them unnecessarily or not completing the prescribed course can lead to antibiotic resistance. This means that antibiotics may become less effective at treating UTIs and other infections over time.
- Recurrent UTIs and Antibiotic Use: Some women experience recurrent UTIs and may require multiple rounds of antibiotics. While antibiotics are effective at treating each UTI episode, repeated use may increase the risk of antibiotic resistance.
- Probiotics and UTIs: Probiotics are “good” bacteria that may help maintain a balanced gut and urinary tract microbiome. This balance may make it more challenging for harmful bacteria to take hold, potentially reducing the frequency of UTIs.
Antibiotics play a vital role in treating UTIs, but their overuse can lead to antibiotic resistance, which is a growing concern. It’s essential to use antibiotics judiciously, complete prescribed courses, and explore preventive measures to minimise the risk of UTIs.
When to Seek Help for UTIs
While many urinary tract infections (UTIs) can be managed with over-the-counter remedies, there are situations where seeking a specialist’s help becomes necessary. Here are some scenarios when you should consider consulting a specialist for your UTI:
- Recurrent UTIs: If you experience multiple UTIs within a short period, typically defined as three or more in a year, it’s advisable to consult a doctor, urologist or urogynecologist. They can assess your condition more comprehensively, investigate underlying causes, and recommend specialised treatments or preventive measures.
- Complicated UTIs: Complicated UTIs occur when factors such as structural abnormalities in the urinary tract, urinary tract stones, or other medical conditions complicate the infection. In these cases, a specialist like a urologist can provide expert evaluation and tailored treatment plans.
- Persistent or Severe Symptoms: If your UTI symptoms persist despite treatment or become severe, involving symptoms like high fever, kidney pain, or blood in the urine, consult a specialist. These symptoms may indicate a more severe infection, such as a kidney infection, or complications that require immediate attention.
- Complications or Unusual UTIs: If you experience uncommon or complicated UTIs, such as kidney infections (pyelonephritis) or infections caused by antibiotic-resistant bacteria, a specialist can help determine appropriate treatment options and address any underlying issues.
- UTIs During Pregnancy: UTIs require special care, as they can pose risks to the mother and the baby. Pregnant women with UTIs should consult an obstetrician-gynaecologist (OB-GYN) for safe and effective management.
- Underlying Health Conditions: If you have underlying health conditions that may increase your susceptibility to UTIs or complicate their treatment, such as diabetes or a weakened immune system, a specialist can provide specialised care and recommendations tailored to your unique medical circumstances.
- Chronic UTI Symptoms: Chronic UTI symptoms, which may persist for an extended period or recur frequently, should be evaluated by a specialist. A doctor can perform in-depth assessments to identify potential underlying causes and develop targeted treatment strategies.
In all of these situations, seeking the expertise of a healthcare provider can help ensure you receive the most appropriate and effective care for your UTI. Specialists can conduct thorough evaluations, offer advanced diagnostic tests, and provide specialised treatment plans when needed, ultimately improving your chances to prevent urinary tract infections and reduce your risk of recurrent infections.